Case Report
Efficacy of early Hyperbaric Oxygen Therapy in Central Retinal Artery Occlusion

Ayse Gul Kocak Altintas* and Mehmet Citirik
SB Ankara Ulucanlar Eye Training and Research Hospital, Turkey
*Address for Correspondence: Ayse Gul Kocak Altintas, Medical Doctor-Associated Professor, Ulucanlar Cad. No: 5906230 Altindag, Ankara, Turkey, Tel: 90-312-3126261, Fax: 90-312-3124827; Email: [email protected]
Dates: Submitted: 31 May 2017; Approved: 19 June 2017; Published: 20 June 2017
How to cite this article: Altintas AJK, Citirik M. Mitomycin-C Use and Complications in Ophthalmology. Int J Clin Exp Ophthalmol. 2017; 1: 023-028. DOI: 10.29328/journal.ijceo.1001003
Copyright Licence: © 2017 Altintas AGK, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Central retinal artery occlusion; Early treatment; hyperbaric oxygen
Abstract
A 60-year-old woman had central retinal artery occlusion (CRAO) presented to the ophthalmology department with a sudden, painless loss of vision. Her initial visual acuity was light perception and she treated with hyperbaric oxygen therapy (HBOT) 4 hours after the development of visual symptoms. Systemic risk factors were not found so she was diagnosed as having idiopathic CRAO. Her vision improved from light perception to 20/50 after the HBOT. Any complications such as neovascularization were not developed until the last follow up visit of 8th months.
Introduction
Central retinal artery occlusion (CRAO) is an important vascular cause of profound vision loss caused by partial or complete occlusion of the central retinal artery. Due to the high risk of this severe permanent visual impairment, timely diagnosis and effective emergency treatment is needed to prevent the onset of irreversible complications. Hyperbaric oxygen therapy (HBOT) has been used to treat patients with CRAO and most of treated cases have shown improvement [1-4]. Aggressive management with ocular massage, anterior chamber paracentesis without urgent HBOT does not appear to improve visual acuity. Irreversible retinal destruction occurs in a little while after the central retinal artery obstruction. Hayreh and Jonas [5], suggested that CRAO lasting more than 240 minutes causes permanent retinal damage with gliosis formation and optic nerve atrophy in Rhesus monkeys. Hattenbach and coworkers [6], observed that visual outcome was better in patients treated within 6.5 h period after the onset of CRAO, comparing to others treated between 6.5 and 12 h after the vision loss.
Case Report
A 60-year-old woman presented to the ophthalmology hospital complaining of sudden visual loss in her left eye. She reported of marked painless vision loss since 07.30 am in the morning when she woke up. On ocular examination at 08.30 am, when she came to emergency department of eye hospital, her visual acuity in the left eye was only light perception and a relative afferent pupillary defect was observed in same side. The best corrected visual acuity was 20/20 on her right eye. Conjunctiva, corneal transparency, anterior chamber, and crystalline lens were normal on both sides. Intraocular pressure was 14 mm/Hg and 16 mm/Hg on right and the left eye respectively. Fundus examination revealed, disruption of the arteriolar blood supply of the retina, a pale and edematous retina mainly located in posterior pole combining with macular cherry-red spot leading to a diagnosis of central retinal artery occlusion. Her right fundus was normal.
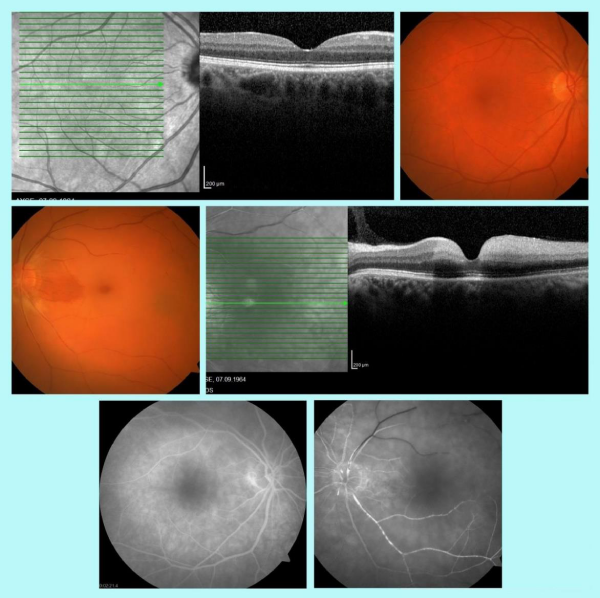
A conservative treatments, including reducing intra-ocular pressure with systemic carbonic anhydrates inhibitor (acetazolamide), intravenous mannitol1.5-2 g/kg over 60 minute and ocular massage on her left eye was applied between further ophthalmologic examinations including color fundus imaging, fundus Fluorescein Angiography (FFA Topcon, Tokyo, Japan) and spectral domain optical coherence tomography (OCT) imaging (Heidelberg, Heidelberg, Germany) tests during 1 and a half hour period in initial visit. FFA showed an increased arm-retina time, delayed and incomplete filling in the central retinal artery in affected eye comparing to contralateral side (Figure 1). OCT evaluation revealed diffuse edema involving both inner and outer retina with loss of the foveal contour (Figure 1). Before comprehensive systemic evaluation, she was send to urgent hyperbaric oxygen (HBO) treatment, and received first session of 100% oxygen 3 hour after her admitted to hospital and 4 hours after beginning of her visual symptoms. She was scheduled for treatment by a daily session of 2 h of HBO at 2.5 atmospheres absolute for 20 days.
She denied headache or any associated neurologic complaints and history of ischemic stroke or prior hypercoagulable state. To evaluate the ethological factors she was sent to a hematology consultation to complete hematological screening such as blood count (CBC), serum coagulation tests, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), Fibrinogen level, antiphospholipid antibodies, prothrombin time (PT), activated partial thromboplastin time (aPTT), serum protein for coagulopathies,. Also, cholesterol, triglycerides, and lipid panel to evaluate for atherosclerotic disease and blood cultures for bacterial endocarditis and septic emboli were done. Hematological investigations were normal and autoantibody screening was negative. Echocardiography and carotid Doppler ultrasonography results were normal. The risk factors for a CRAO and acute cerebral ischemia or lacunar infarctions are very similar so brain magnetic resonance imaging (MRI) test was performed. A detailed neurological evaluation and MRI results were also normal. Systemic evaluation revealed that she was not having diabetes, hypertension, atherosclerosisor any other systemic disease. According to these comprehensive systemic examination results she diagnosed to have an idiomatic CRAO.
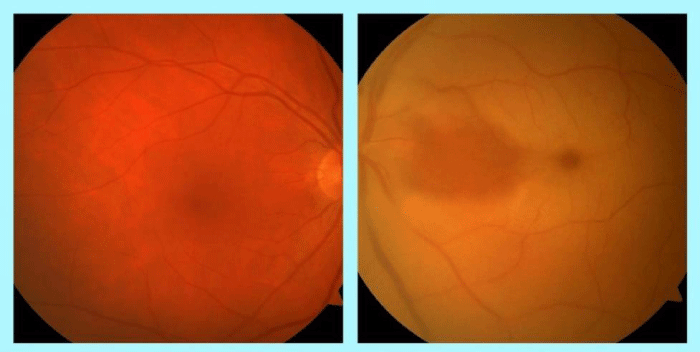
The patient was scheduled for a regular follow-up. At the 1 week follow-up, her vision increased to 1meter finger counting and the central scotoma was disappeared. In the left eye, the disc boundary was clear and pale, cherry-red spot disappeared, even the retinal edema had resolved remarkably on the temporal side of macula it was still persist in the maculae papillary bundle when she was undergoing HBO treatment (Figure 2).
At the 1-month follow-up, visual acuity increased to 20/100in the effected eye, the fundus examination revealed the optic disc was pale, retina arteriolar narrowing was persisted and the peripheral retina was normal. The central retinal edema had disappeared but the macular pigment was mildly disordered. The central macular thickness was decreased comparing to fellow eye which was 158µ to 245 µin left and right eye respectively. The fundus examination was normal in the right eye.
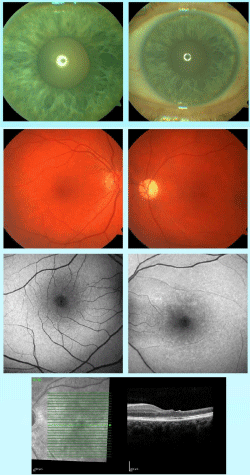
At the 2-month visual acuity increased to 20/50. Fundus finding were the same except macular thickness was increased to186 µ which continued to increase204 µ until month 3 and the thinning of inner retinal layers partially recovered.
At the 6-month follow-up the visual acuity remained in 20/50, optic disc was still pale, retina was normal except the central retinal artery was partially sclerosed and narrowing of arterioles were still persisted. The central macular thickness reached to 205 µ (Figure 3).
The patient was followed regularly for the development of retinal, iris and optic nerve neovascularization as CRAO complications. At the latest visit of 8 month each ophthalmic findings were the same without any complications (Figure 3).
Discussion
CRAO is an ophthalmic emergency and the ocular analogue of cerebral stroke. Best evidence reflects that over three-quarters of patients suffer profound acute visual loss with a visual acuity of 20/400 or worse. This results in a reduced functional capacity and quality of life [1]. Acute treatment for maintain visual acuity is usually effective within limited times. Hayreh and Jonas [5], reported that complete or almost total optic nerve atrophy and nerve fiber damage were present in all eyes in which the duration of central retinal artery occlusion was 240 minutes or more. Hattenbach and coworkers [6], declared that thrombolytic treatment with intravenous low-dose recombinant tissue plasminogen activator is of value for an improved visual recovery in patients with acute CRAO, if administered within the first 6.5 hours after the onset of symptoms.
On the other hand result of several reports has shown that HBOT within 24-48 hours after the inciting event, had impressive improvement of visual acuity, while the retinal ischemia is still reversible. Paul et al defined that completeness of retinal artery occlusion could be more important than relationship between the time from onset of symptom to initiation of treatment [7]. Ahn et al. [8], showed that clinically significant visual acuity improvement was observed in 76.9% of eyes with incomplete CRAO occlusion while visual recovery was not observed in any subjects with total occlusion. Schmidt et al. [9], showed similar outcome that 50% of patients who treated with intra-arterial thrombolysis (IAT) for incomplete occlusion had significant improvement in visual acuity compared to 0% of patients with a total occlusion.
As far as we know our case was the most successfully treated patient in term of improvement in visual function. Lemos et al. [10], reported a patient with initial VA of 20/400 had a marked improvement in vision after HBOT and increased to 20/32. Although the final VA of their patient was higher than that of our patient the initial VA was also much higher than ours which was an indirect evidence of better initial retinal function. Simental [11], reported an 11 year- old patient presented with a visual acuity of light perception and a relative afferent pupillary defect due to hemiretinal artery occlusion. Even the initial visual function of their patient was very similar to ours, he had recovered to vision of 20/200 which was lower than our patient’s post treatment VA. In addition, he had only hemiretinal artery occlusion while our patient had central retinal artery occlusion which affected larger retinal area.
Our case was treated with urgent HBOT which started in 4 hours after the initial symptoms, partially reperfusion was occurred in occluded artery and visual function significantly improved in a four weeks then continued to increase and finally reach to 20/50.
The inner two-thirds of retina normally supplies by central retinal artery perfusion. It also receives oxygen from the choroidal vasculature which supplies the outer one-third of retina. Intermittent breathing of 100% oxygen under 2.5 atmospheres in HBOT, as our treatment algorithm for retinal artery occlusion, can increase the amount of oxygen dissolved in plasma, from 0.32 to 6 mL O2/100 mL which is almost 17-fold than breathing room air. This high level of dissolved plasma oxygen from the choroidal circulation can diffuse in to the inner layers of the retina, without the need for hemoglobin, to maintain its function until the central retinal artery recanalizes and recovery of its perfusion [12-15]. In our patient both effective emergency treatment with HBO and developing re-perfusion in occluded CRA, with the help of physical dislocation of the central obstruction by ocular massage and reduction of intraocular pressure, may cause achievement in vision recovery and preventing long term complications.
In complete retinal arterial occlusions retinal whitening occurs due to stasis of axoplasmic flow and intracellular edema in the inner retinal layers which can be seen as increased reflectivity on OCT of the inner retinal layers. If re-perfusion does not occurs, retinal atrophy progressed over several months, in which the reflectivity progressively disappeared in a 4-6 weeks period due to subsequent death of retinal cells mainly neuronal cells and development of gliosis and acellular scar of the inner retinal layers, despite relative sparing of the cells in outer retinal layers. On this period OCT findings shows thinning of the inner retina due to irreversible retinal damage [15-16]. We observed edema in inner retinal layer which was more prominent in nasal part of the maculae in acute period which was disappeared later on and macular thickness decreased during the first month when she was receiving HBOT, then continued to increase until month 3 and finally stabilized on follow-up visits. Even CMT was lower than that of following eye, according to OCT analyses the internal structure of nasal retina remained undisrupted. This progressive OCT results were indirect evidence that partial revitalization of retinal continued after completion of HBOT.
Patients had CRAO need to be followed more closely for both the development of complications such as neovascularization on optic nerve, retina and rubeozis iridis [17-18]. Until the latest follow up of 8th months any complication did not observed.
To find out risk factors of occlusion and to prevent another potential attack an extensive systemic evaluation must be done. The CRAO mostly occurred by an embolus from the ipsilateral carotid artery, aortic arch or heart. It is generally related with any other systemic diseases such as cardiac and hematological disorders but can also be idiopathic such as our patient. After extensive systemic evaluation we could not found any related risk factors. Because of similar situations in the framework of retina and brain, further research about pathology of the microvasculature of the brain may help to give correct diagnosis of patient that can be consider as an idiopathic CRAO nowadays. Due to the risk of permanent visual loose and high frequency of complications in CRAO correct diagnosis and effective emergency treatment needed.
References
- Varma DD, Cugati S, Lee AW, Chen CS. A review of central retinal artery occlusion: clinical presentation and management. Eye (Lond). 2013; 27: 688-697. Ref.: https://goo.gl/oodypE
- Hayreh SS, Zimmerman MB. Fundus changes in central retinal artery occlusion. Retina. 2007; 27: 276-289. Ref.: https://goo.gl/sxMUjF
- Hayreh SS, Zimmerman MB, Kimura A, Sanon A. Central retinal artery occlusion. Retinal survival time. Exp Eye Res. 2004; 78: 723-736. Ref.: https://goo.gl/m63EaS
- Hayreh SS, Zimmerman MB. Central retinal artery occlusion: visual outcome. Am J Ophthalmol. 2005; 140: 376-391. Ref.: https://goo.gl/zx8LkM
- Hayreh S, Jonas JB. Optic disk and retinal nerve fiber layer damage after transient central retinal artery occlusion: an experimental study in rhesus monkeys. Am J Ophthalmol. 2000; 129: 786-795. Ref.: https://goo.gl/YSZf9D
- Hattenbach LO, Kuhli-Hattenbach C, Scharrer I, Baatz H. Intravenous thrombolysis with low-dose recombinant tissue plasminogen activator in central retinal artery occlusion. Am J Ophthalmol. 2008; 146: 700-706. Ref.: https://goo.gl/mxBdfy
- Page PS, Cambon AC, James RF. Visual improvement after intra-arterial thrombolysis for central retinal artery occlusion does not correlate with time to treatment. Interv Neurol. 2016; 5: 131-139. Ref.: https://goo.gl/8FZWGp
- Ahn SJ, Kim JM, Hong JH, Woo SJ, Ahn J, et al. Efficacy and safety of intra-arterial thrombolysis in central retinal artery occlusion. Invest Ophthalmol Vis Sci. 2013; 54: 7746-7755. Ref.: https://goo.gl/GFqFb4
- Schmidt DP, Schulte-Monting J, Schumacher M. Prognosis of central retinal artery occlusion: local intraarterial fibrinolysis versus conservative treatment. AJNR Am J Neuroradiol. 2002; 23: 1301-1307. Ref.: https://goo.gl/7L6rpj
- Lemos JA, Teixeira C, Carvalho R, Fernandes T. Combined central retinal artery and vein occlusion associated with factor v leiden mutation and treated with hyperbaric oxygen. Case Rep Ophthalmol. 2015; 6: 462-468. Ref.: https://goo.gl/shh4Y1
- Simental DEA, RoigMelo-Granados EAR, Quezada SC, Escamilla MAP, Orozco CLS, et al. Hemiretinal Artery Occlusion in an 11-Year-Old Child with Dextrocardia. Case Rep Ophthalmol Med. 2016; 2016: 5104789. Ref.: https://goo.gl/j8savH
- Dattilo M, Biousse V, Newman NJ. Update on the Management of Central Retinal Artery Occlusion. Neurol Clin. 2017; 35: 83-100. Ref.: https://goo.gl/XKQivT
- Gilbert AL, Choi C, Lessell S. Acute management of central retinal artery occlusion. Int Ophthalmol Clin. 2015; 55: 157-166. Ref.: https://goo.gl/S7dZdD
- Murphy-Lavoie H, Butler F, Hagan C. Central retinal artery occlusion treated with oxygen: a literature review and treatment algorithm. Undersea Hyperb Med. 2012; 39: 943-953. Ref.: https://goo.gl/hWRKsH
- Olson EA, Lentz K. Central retinal artery occlusion: a literature review and the rationale for hyperbaric oxygen therapy. Mo Med. 2016; 113: 53-57. Ref.: https://goo.gl/Sm8Jcp
- Oguz H, Sobaci G. The use of hyperbaric oxygen therapy in ophthalmology. Surv Ophthalmol. 2008; 53: 112-120. Ref.: https://goo.gl/Jvi6gF
- Tang PH, Engel K, Parke DW. Early onset of ocular neovascularization after hyperbaric oxygen therapy in a patient with central retinal artery occlusion. Ophthalmol Ther. 2016; 5: 263-269. Ref.: https://goo.gl/VUTXuK
- Rudkin AK, Lee AW, Chen CS. Ocular neovascularization following central retinal artery occlusion: prevalence and timing of onset. Eur J Ophthalmol. 2010; 20: 1042-1046. Ref.: https://goo.gl/VinSUC