More Information
Submitted: 07 January 2020 | Approved: 28 January 2020 | Published: 29 January 2020
How to cite this article: Ireju Onyinye Chukwuka, Chinyere Nnenne Pedro-Egbe. Demographic pattern of refractive anomalies in Niger Delta presbyopes-Implications for preventive eye care practice. Int J Clin Exp Ophthalmol. 2020; 4: 005-008.
DOI: 10.29328/journal.ijceo.1001025
Copyright Licence: © 2020 Ireju Onyinye Chukwuka, Chinyere Nnenne Pedro-Egbe. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Refractive anomalies; Presbyopia; Port Harcourt; Nigeria
Demographic pattern of refractive anomalies in Niger Delta presbyopes - Implications for preventive eye care practice
Ireju Onyinye Chukwuka* and Chinyere Nnenne Pedro-Egbe
Department of Ophthalmology, College of Health Sciences, University of Port Harcourt, Nigeria
*Address for Correspondence: Ireju Onyinye Chukwuka, Department of Ophthalmology, College of Health Sciences, University of Port Harcourt, Nigeria, Tel: +234-8033103817; Email: [email protected]; [email protected]
Background/Aim: In spite of global initiatives to provide sight for all by the year 2020, many middle-aged to elderly people in the Niger Delta still have significant visual impairment due to uncorrected refractive errors. The aim of this study is to assess the types of refractive anomalies that occur among presbyopic patients in Port Harcourt and determine the demographic pattern of these anomalies based on age and gender characteristics.
Methodology: This is a hospital-based descriptive cross-sectional study in which sixty consecutive adult patients for refraction were seen. Every adult patient that came to get glasses during the study period was included in the study except where ocular or systemic contraindications were present. In addition to visual acuity, all patients had a detailed ocular examination and then refraction. The collected data was subsequently analysed using SPSS version 20.
Results: The mean age of the patients was 54.4 ± 9.4 years with a range of 35 to 80 years. A total of 60 patients were seen, comprising 30 males and 30 females. The commonest refractive error was presbyopia with hyperopic astigmatism and this accounted for 80% of all cases. Hyperopic presbyopia and presbyopia alone were the least common.
Conclusion: There is a high level of cylindrical and spherical errors in Port Harcourt. The full optical correction should always be prescribed to presbyopic patients to fully correct the associated visual impairment and improve the patients’ well-being.
Worldwide, uncorrected refractive error is the main cause of moderate and severe visual impairment and the second leading cause of blindness [1], accounting for an estimated 153 million and 8 million affected persons, respectively, despite the fact that correction of refractive error with appropriate spectacles is one of the most cost-effective interventions in eye health [2].
Refractive error is a complex and multifactorial condition that varies in prevalence across populations with different genetics, demographics, ocular and extrinsic factors, such as education. The Nigerian National Blindness and Visual impairment Survey [3] indicated that uncorrected refractive error accounts for 57.1% of moderate visual impairment (visual acuity [VA], > 6/18–6/60). Economic consequences are considerable, as uncorrected refractive errors including presbyopia also affect people in the working-age group. Presbyopia is the type of refractive error which occurs due to loss of elasticity of the lens capsule and lens substance; it’s an age-related change and is common all over the world. This article reports on the types of refractive error that occur among patients in the presbyopic age group (35 to 80 years) in Port Harcourt, located in the Niger Delta region of Nigeria. To the best of our knowledge, no such study has been conducted in this locality before for comparison with results from other parts of the country.
A hospital-based descriptive cross-sectional study was used. Using the Cochrane’s formula for sample size based on the following parameters: an alpha-level of 0.05, prevalence of refractive anomalies of 15.8% [1] precision level of 0.1, and a non-response rate of 10%, a sample size of 56 was attained. This was rounded off to 60.
Sixty patients with refractive anomalies were recruited into the study within a period of four weeks. Each subject had to be at least thirty-five years old but they were excluded from the study if they had uncontrolled Hypertension/Diabetes or had significant ocular pathology like advanced pterygia/advanced cataract or other intraocular inflammatory conditions. The baseline information was obtained for each subject including age, gender, a history of ocular or systemic comorbidity, ocular surgeries, previous use of glasses and when the last pair was obtained and family history of refractive error/other ocular or systemic disease. The ocular examination included visual acuity with and without a pinhole, estimation of near vision using a Raynier test type, examination of the anterior segment with a pen torch and funduscopy using a Welch Allyn direct ophthalmoscope. A detailed anterior segment examination was performed with a slit lamp microscope (SL 115 Classic Slit Lamp; Carl Zeiss Meditec AG, Jena, Germany) and intraocular pressure measurement was made using an air-puff tonometer. All participants had non-cycloplegic refraction by an optometrist using an auto-refracto-keratometer (ARKM-100; Takagi Seiko, Japan) that was regularly calibrated and the subjective examination was carefully done with appropriate lenses, Jackson cross cylinders and duochrome test. Cylindrical lenses were only prescribed when the spherical equivalent was not accepted by the patient. All the information was entered into a proforma specifically designed for the study. Data analysis was performed using the IBM Statistical Package for Social Sciences (SPSS) version 20. Frequencies and percentages were used to summarize categorical variables while means and standard deviation were employed for numerical variables. The differences in means were compared using Analysis of Variance (ANOVA). Two-tailed Fisher’s exact test was employed for comparison between proportions. Statistical significance was set at p < 0.05. For the purpose of this study, myopia was defined as a spherical error of > -0.5 diopters (D), hyperopia as spherical error of > +0.50D, and astigmatism as a cylindrical error of > 0.25D.
In the study, a total of 60 patients had refractive anomalies. The mean age of the patients was 54.4 ± 9.4 years with a median of 53 years and a range of 35 to 80 years. The male to female ratio was 1:1, comprising 30 males and 30 females.
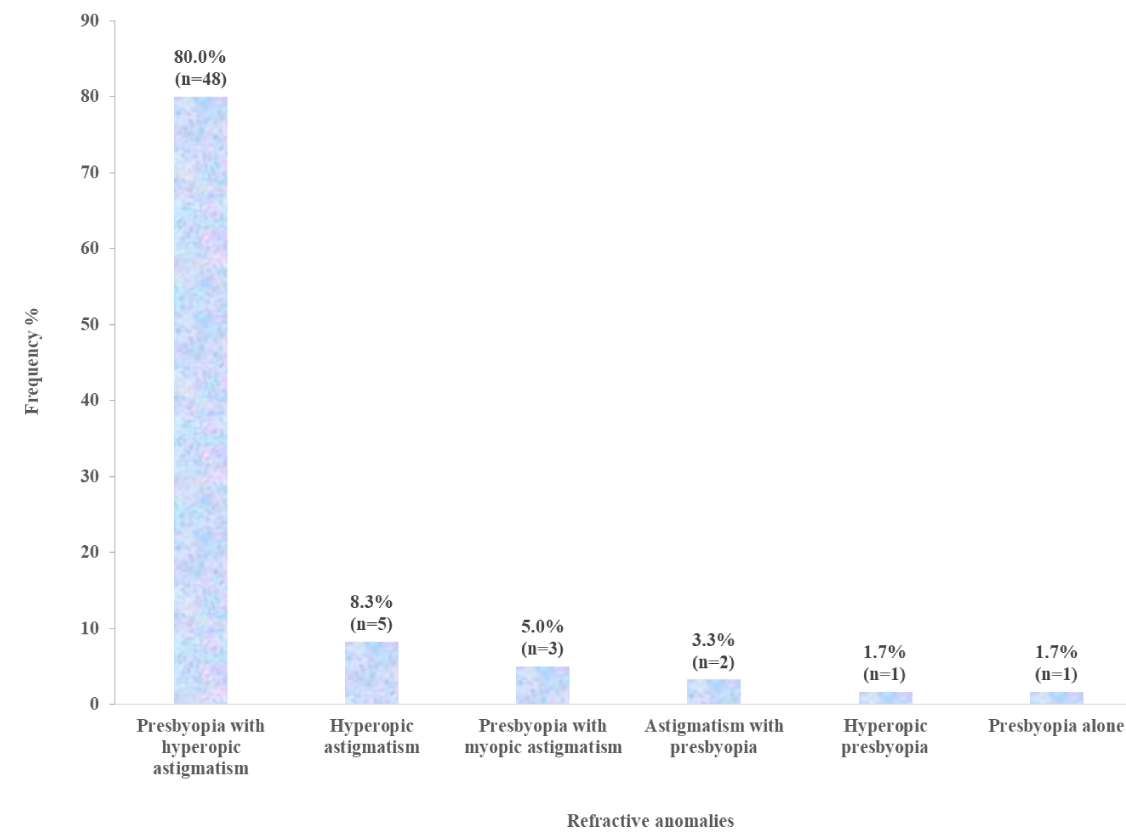
Presbyopia with hyperopic astigmatism was the most common disorder encountered occurring in 80% (n = 48) of subjects and followed by hyperopic astigmatism without presbyopia (n = 5; 8.3%) and presbyopia with myopic astigmatism (n = 3; 5%). Astigmatism was present in 85% of the patients, and only 1.7% had presbyopia alone. Presbyopia was not seen in 8.3% of the study participants.
Distribution of refractive anomalies
Figure 1 shows the distribution of refractive anomalies in the study population. Presbyopia with hyperopic astigmatism accounted for most of the refractive anomalies seen (n = 48; 80%).
Figure 1: Frequency Distribution of Refractive Anomalies.
The relationship between gender and refractive anomalies
In table 1, the proportion of refractive anomalies is compared by gender. It shows that there is a slight female preponderance in hyperopic astigmatism (F:M = 60%:40%) compared to the reverse in presbyopia with myopic astigmatism (F:M = 33.3%:66.7%). For presbyopia with hyperopic astigmatism, both genders are affected to the same degree.
| Table 1: Relationship between Gender and Refractive Anomalies. | |||
| Gender | |||
| Refractive Anomalies | Male n (%) |
Female n (%) |
Total n (%) |
| Hyperopic astigmatism | 2 (40.0) | 3 (60.0) | 5 (100.0) |
| Presbyopia alone | 0 (0.0) | 1 (100.0) | 1 (100.0) |
| Presbyopia with myopic astigmatism | 2 (66.7) | 1 (33.3) | 3 (100.0) |
| Presbyopia with hyperopic astigmatism | 24 (50.0) | 24 (50.0) | 48 (100.0) |
| Hyperopic presbyopia | 0 (0.0) | 1 (100.0) | 1 (100.0) |
| Astigmatism with presbyopia | 2 (100.0) | 0 (0.0) | 2 (100.0) |
| Total | 30 (50.0) | 30 (50.0) | 60 (100.0) |
| Fisher’s exact = 4.176; p - value = 0.748 | |||
The relationship between mean age and refractive anomalies
Table 2 shows that a combination of presbyopia with either myopia, hyperopia or astigmatism was commoner in those who were aged 55 years or older and this was statistically significant (p = 0.049).
| Table 2: Comparison of mean ages of patients across type of refractive anomaly. | ||
| Refractive Anomalies | N | Mean Age ± SD (years) |
| Hyperopic astigmatism | 5 | 42.80 ± 8.11 |
| Presbyopia alone | 1 | 42.00 ± 0.00 |
| Presbyopia with myopic astigmatism | 3 | 57.33 ± 12.70 |
| Presbyopia with hyperopic astigmatism | 48 | 55.27 ± 8.80 |
| Hyperopic presbyopia | 1 | 61.00 ± 0.00 |
| Astigmatism with presbyopia | 2 | 56.50 ± 3.54 |
| ANOVA = 2.395; p - value = 0.049*; *Statistically significant | ||
The two main findings from this study are the extremely high percentage of patients with different types of astigmatism (85%) and the commonest refractive error being presbyopia with hyperopic astigmatism. This outpatient clinic offers free medical services to serving and retired staff of an oil refining company, their spouses and children of currently serving staff under the age of twenty-one years, so young employees without severe ocular symptoms come in lower numbers and being in the productive age bracket would prefer not to be absent from work just for the purpose of getting corrective lenses.
Being hospital based, the study has the inherent limitation of hospital based studies which include selection bias, poor recording systems and inconsistent data sources. The selection bias results from the fact that only those with a subjective awareness of the visual problem will present for examination. Also, the numbers recorded may be increased due to indiscriminate use of the facility because its free (including in this setting patients being entitled to another pair of glasses two years after the last pair was dispensed). To add to these, record keeping and filing systems can be of concern in health facilities in developing countries. However, in spite of these limitations, the results of the present study can be used for planning refractive error services and evaluating the company’s free eye care services.
The pattern of refractive error varies according to population characteristics such as, age, gender, race and ethnicity. Recent reports suggest that the differences in prevalence rates may be attributed to educational pressures, literacy standards and lifestyle changes which tend to vary in urban and rural environments. As refractive errors are a major contributor of mild to moderate impairment of vision, assessment of their relative proportion is essential in strategic planning of health programmes. Chinawa [4], evaluated the impact of presbyopia among teachers in public schools in rural communities in Rivers State and discovered that sixty-six (66%) out of one hundred teachers had presbyopia and 57.6% of them reported that their duties were adversely affected by uncorrected presbyopia.
Abah [5] in a study of the profile of refractive errors and presbyopia in the Ahmadu Bello university community found that 49.7% of patients over the age of 40 years had presbyopia and the commonest refractive errors in their series were astigmatism and myopia. Hashemi, et al. [6], in the systematic review of refractive systems across the world showed that astigmatism was the most common refractive error in children and adults followed by hyperopia and myopia and this is in line with our findings here. McCarty [7], observed that myopia prevalence rate strongly correlates with the rate of uncorrected refractive error suggesting that myopia could be responsible for much of the uncorrected refractive errors in the world [3,6] but hospital-based studies on refractive errors have been carried out in different geographical locations in Nigeria and the national blindness and visual impairment survey revealed a much lower prevalence of myopia in Nigeria than expected (9.4%)). Malu, et al. [8], while reviewing presbyopes in Plateau state, Nigeria observed that plano presbyopia which decreased with increasing age was the commonest presentation, followed by hyperopic presbyopia which increased with increasing age. She also reported that myopic presbyopia was uncommon. Koroye-Egbe, et al. [9], in Bayelsa state, Southern Nigeria, found astigmatism to be the commonest refractive error and it was seen in 45.63% of patients.
There is a definite gender bias in most of the results in Nigeria. All the results from studies done in the Northern states/region show that more males than females were corrected for refractive error while most of the studies from the southern states show that more females than males were corrected for refractive error [5,8,10,11]. We believe that the ‘apparently’ higher incidence of refractive errors in northern males is due to the restrictions on northern women due to Islamisation and much reduced numbers of girl-child education. In this series as was the case with Chinawa’s result which incidentally was obtained from rural settings in this state, there was no preponderance of either gender but the differences in the mean ages by type of refractive anomaly was significant here(p < 0.05). Lower mean ages were reported among patients with hyperopic astigmatism and presbyopia alone, while those with hyperopic presbyopia and presbyopia with myopic astigmatism had higher mean ages. (p = 0.049). Similar to our findings, in a one-year study at the Aminu Kano University Teaching Hospital Kano, Lawan [10], reported that presbyopia alone accounted for 17% of the presbyopic prescriptions while the remaining 83% required associated distance correction. In Ogun state, Southwest Nigeria Bogunjoko, et al. [11], in a five-year retrospective study of 1000 patients also found astigmatism to be the commonest cause of refractive error in adults (64.8%), followed by hyperopia (21.5%) and myopia (13.7%) and the mean age was 48.2 years. The observation that 90% of all the patients seen in this study had another refractive error besides presbyopia justifies the belief that most older patients in resource poor settings are handicapped by visual impairment, have ocular induced reduction in productivity and quality of life [11,12] and are prone to falls and accidents. This then perpetuates the poverty cycle and may result in over-dependence on family members, isolation and depression. They usually rely on free readers prescribed at eye camps or bought from the local market and even when a proper refraction is done and they get bifocals, they erroneously only use them when they want to read.
Sustained advocacy is necessary to bridge the knowledge gap. It might become necessary to advice donors against the distribution of free readers at eye camps to bring to the fore the magnitude of the problem. Instead all primary health centres should provide easy access to refraction services and be able to dispense good quality, highly subsidised bifocals by partnerships of governments/policy makers with NGOs. With the large number of registered Optometrists in Nigeria, this is sustainable.
Finally, uncorrected refractive error including presbyopia is a global challenge that is keeping us from meeting the World Health Organisation’s Vision 2020 Millennium development goals [13]. We need to re-strategize by urgent and intense advocacy with ocular health education beginning from the grassroots [6]. Politicians, policy makers, primary care providers, and eye specialists need to work together to develop simple, creative strategies to combat visual impairment caused by uncorrected refractive errors. The published data can serve as a baseline to compare the success of earlier interventions. The time to act boldly is now, as we accept our shortfalls and await the announcement of another year for actualisation of our Millennium development goals ….2030 or even 2040?
- Foster A, Resnikoff S. The impact of Vision 2020 on global blindness. Eye. 2005; 19: 1133-1135. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16304595
- Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008; 86: 63-70. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18235892
- Ezelum C, Razavi H, Sivasubramaniam S, Gilbert CE, Murthy GV, et al. Nigeria National Blindness and Visual Impairment Study Group. Refractive Error in Nigerian Adults: Prevalence, Type, and Spectacle Coverage. Invest Ophthalmol Vis Sci. 2011; 52: 5449-5456.
- Chinawa NE, Pedro-Egbe CN, Ejimadu CS. The Impact of Presbyopia among teachers in Public schools in Rural communities in Rivers State and the benefits of Prebyopic correction. Int J Med Medical Sci. 2016; 3: 169-172.
- Abah ER, Chinda D, Samaila E, Anyebe EE. Profile of refractive errors and presbyopia in a university community: A clinical study. Ann Nigerian Med. 2010; 4: 55-58.
- Hashemi H, Akbar F, Abbasali Y, Reza P, Hadi O, et al. Global and Regional Estimates of Prevalence of Refractive Errors: Systematic Review and Meta-analysis. J Current Ophthalmol. 2018; 30: 3-22.
- McCarty CA. Uncorrected refractive error. Br J Ophthalmol. 2006; 90: 521-522.
- Malu KN. Presbyopia in Plateau state, Nigeria: A hospital study. J Med Tropics. 2013; 15: 151-155.
- Koroye-Egbe A, Overensi-Ogbomo G, Adio A. Refractive error status in Bayelsa State, Nigeria. J Nigerian Optometric Association. 2010; 16: 11-6.
- Lawan A, Okpo E, Philips E. Refractive errors in Presbyopic patients in Kano. Annals of African medicine. 2014; 13: 21-24. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24521573
- Bogunjoko TJ, Hassan AO, Anene CI, Ogbonna IJ. Refractive error patterns at a community eye hospital in Southwest of Nigeria. Int J Information Res Rev. 2017; 4: 4334-4338.
- Bekibele CO, Gureje O. Impact of self-reported visual impairment on quality of life in the Ibadan study of ageing. Br J Ophthalmol. 2008; 92: 612-615. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18296505
- Patel I, Munoz B, Burke AG, Kayongoya A, McHiwa W, et al. Impact of presbyopia on quality of life in a rural African setting. Ophthalmology. 2006; 113: 728-734. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16650665