More Information
Submitted: 08 January 2020 | Approved: 24 February 2020 | Published: 25 February 2020
How to cite this article: Siddappa SN, Mahalingu DS, Anjenappa R, Joy TS. Two different patterns and outcome of neodymium YAG capsulotomy. Int J Clin Exp Ophthalmol. 2020; 4: 012-014.
DOI: 10.29328/journal.ijceo.1001027
Copyright Licence: © 2020 Siddappa SN, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Two different patterns and outcome of neodymium YAG capsulotomy
Sudeep Navule Siddappa*, Darshan Shivaura Mahalingu, Rakesha Anjenappa and Tintu Susan Joy
Department of Ophthalmology, Hassan Institute of Medical Sciences, Hassan, Karnataka, India
*Address for Correspondence: Sudeep Navule Siddappa, Department of Ophthalmology, Hassan Institute of Medical Sciences, Hassan, Karnataka, India, Tel: +91 7975077601; 7411490633; Email: [email protected]
Visual impairment is a global health problem. Cataract is responsible for 50% of blindness worldwide [1].
Posterior capsular opacification is the most common late complication of cataract surgery as a result of proliferation of residual lens epithelial cells overall 25% of patients undergoing extra-capsular cataract surgery develops visually significant PCO within 5 years of the operation [2].
Nd: YAG laser provides the advantage of cutting the posterior lens capsule, thereby avoiding and minimizing infection, wound leaks, and other complication of intraocular surgery. Thus Nd:YAG laser capsulotomy is noninvasive, effective and relatively safe technique [3].
However, this procedure is associated with complications such as- postoperative increased intraocular pressure (IOP), cystoid macular edema (CME), disruption of the anterior vitreous surface, uveitis, lens subluxation, increased incidence of retinal detachment and pitting of the IOL [4].
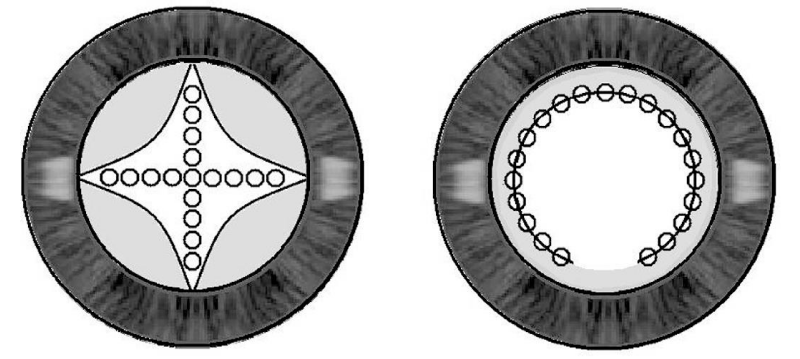
Laser shots can be applied in several patterns such as “Cruciate or Cross pattern”, “Can opener”, inverted “U-Method” and in a “Circular pattern”. Many authors promote the use of a cruciate pattern in the Centre of the visual axis, with the clinician starting off on both axes away from the Centre to avoid pitting the lens centrally [5].
This study mainly aims to analyze the effect of various forms of PCO capsulotomy openings on visual function after Nd: YAG capsulotomy.
Source of data
The materials for the present study drawn from patients attending the outpatient department of ophthalmology. After considering the below criteria, patients were selected into the study.
Inclusion criteria
All patients presented with diminution of vision due toposterior capsular opacity,
1. Evident posterior capsular thickening/opacification on examination with slit lamp.
2. Post-op cataract surgery, decrease in vision by at least 3 lines on Snellen’s chart.
3. At least 3 months interval between cataract surgery and development of posterior capsular opacification.
4. PCO following complicated cataracts.
5. Pre-existing posterior capsular opacification (present before cataract surgery).
Exclusion criteria
Following patients will be excluded from the study:
1. Patients < 5 years age.
2. Eyes with subluxated intraocular lens.
3. Includes severe coexisting ocular disease,
Glaucoma
Corneal opacity
Diabetic retinopathy
Age-related macular degeneration and other macular pathologies.
Retinal detachment
4. Un-co-operative subjects. Eg: patients with mental retardation, neurological problems.
5. Aphakic eyes.
Methodology
Study was initiated after obtaining approval from the Institutional Ethics Committee,Study conducted in about 100 PCO patients fulfilling the inclusion criteria after obtaining the informed consent from the participants are subjected to-
• A detailed clinical history includes date of cataract surgery, interval between cataract surgery and onset of defective vision, history of glaucoma, history of any systemic illnesses or surgery, history of any other ocular conditions.
• Detailed examination of both eyes along with general physical examination.
• Visual acuity testing with Snellen’s chart.
• Examination of anterior segment of eye by slit lamp biomicroscopy.
• Measurement of intraocular pressure using applanation tonometer (Perkins).
Examination of posterior segment of eye by ophthalmoscopy (direct and indirect) and +90 D biomicroscopy.
A Q‑switched Nd: YAG laser system (YAG IIplus, Appa swamy, India), with wavelength of 1064 nm and pulse length of < 4 ns (2‑3 ns) was employed for this study. Before starting the procedure, one drop of 4% xylocaine was instilled into the conjunctival cul‑de sac.
The pupils were fully dilated and the aim was to create a capsulotomy of about 4 mm in size.
In cruciate pattern posterior capsulotomy laser shot is first aimed superiorly at near 12 Clock in the location of fine tension lines and progressing downwards towards the 6 o’ clock position, shots are then placed at the edge of the capsule opening, progressing laterally towards the 3 and 9 o’ clock positions. In circular pattern a circle of laser shots put starting from 6 o’ clock position with a diameter of 4-5 mm.
The aiming beamwas focused slightly posterior to the posterior capsule. Theoptical center of the IOL was matched with the centerof the opening. Initial setting of 1mJ and subsequent increase of 0.5 mJ as necessary used to make an opening in the posterior capsule.
Post procedure Tab Acetazolamide 250mg BD, Moxifloxacin with Dexamethasone eye drops QID, Nepafenac eye drops BD depending on the inflammatory response and raised IOP. Antiglaucoma medications were not given prior to capsulotomy to any patient.
Follow up
Patients were visited on first, third and seventh postoperative days, then weekly for two weeks, monthly for two months and on third month. Each visit patients visual acuity, refraction, fundoscopy and IOP were examined and analysed. More frequent follow up visits may be considered in patients with complications.
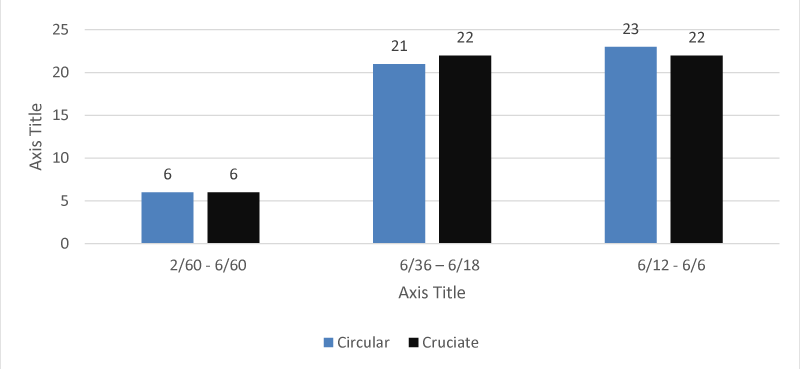
After a study for 18 months Dec 2017- May 2019 the following observations were made, 100 patients were identified having posterior capsular opacity, These patients were divided into group A and group B, group A underwent cruciate and group B underwent circular pattern capsulotomy (Table 1).
| Table 1: Comparison of different pattern of PCO capsulotomy with post laser vision. | ||||
| Pattern of PCO | Post laser vision | Total | ||
| 2/60- 6/60 | 6/36- 6/18 | 6/18-6/6 | ||
| Circular | 6 12.0% |
21 42.0% |
23 46.0% |
50 100.0% |
| Cruciate | 6 12.0% |
22 44.0% |
22 44.0% |
50 100.0% |
| Total | 12 12% |
4 43% |
45 45% |
100 100% |
Graph 1 showing both circular and cruciate pattern capsulotomy have almost same outcome.
Graph 1: Comparison of different pattern of PCO capsulotomy with post laser vision.
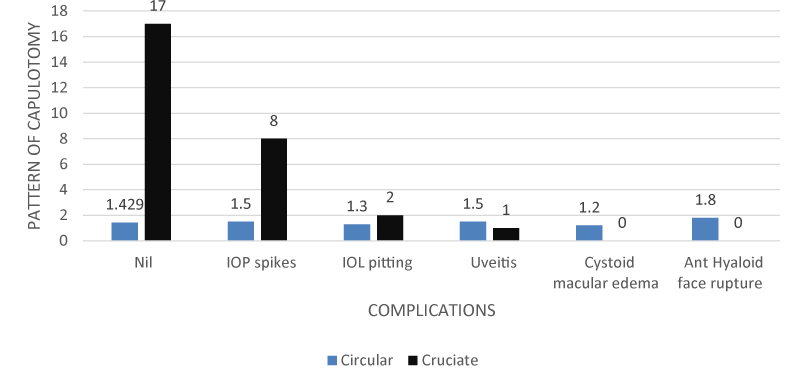
In cases who underwent circular pattern complications like IOL pitting and uveitis are common compared cruciate pattern, where IOP spikes is a common complication (Table 2).
| Table 2: Comparison of different pattern of PCO capsulotomy with complications. | |||
| Complications | Pattern of PCO capsulotomy | Total | |
| Circular | Cruciate | ||
| Nil | 32 47.1% |
36 52.9% |
68 100.0% |
| IOP spikes | 9 45.0% |
11 55.0% |
20 100.0% |
| IOL pitting | 5 83.3% |
1 16.7% |
6 100.0% |
| Uveitis | 3 75.0% |
1 25.0% |
4 100.0% |
| Cystoid macular edema | 1 100.0% |
0 .0% |
1 100.0% |
| Ant Hyaloid face rupture | 0 .0% |
1 100.0% |
1 100.0% |
| Total | 50 50.0% |
50 50.0% |
100 100.0% |
There was a single case of CME found in circular pattern and single case of ant hyaloid face rupture found in patients undergone cruciate pattern of capsulotomy.
Graph 2 showing complication rate is more with the cruciate pattern capsulotomy compared to circular pattern.
Graph 2: Comparison of different pattern of PCO capsulotomy with complications.
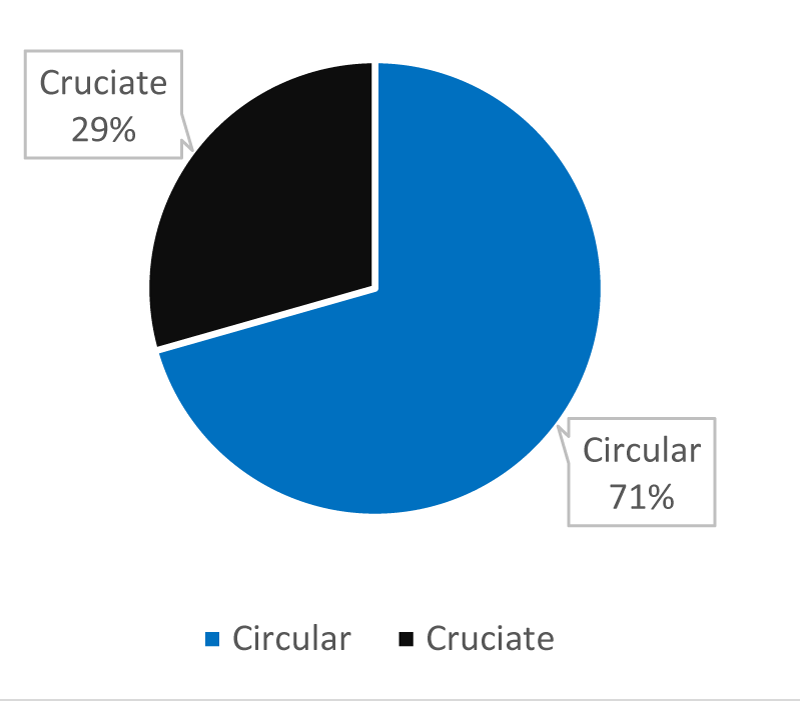
24.5% of cases under gone circular pattern of capsulotomy were complaining of floaters compared to cruciate only 10% (Table 3).
| Table 3: Comparison of different pattern of PCO capsulotomy with floaters. | |||
| Pattern of PCO | Floaters | Total | |
| Yes | No | ||
| Circular | 12 24.5% |
38 75.5% |
50 100.0% |
| Cruciate | 5 10.0% |
45 90.0% |
50 100.0% |
| Total | 17 17.2% |
82 82.8% |
99 100.0% |
This is not statistically significant but cruciate pattern have less chances of floaters compared to circular.
Graph 3 showing circular pattern have higher chances of having floaters compared to cruciate pattern capsulotomy.
Graph 3: Comparison of different pattern of PCO capsulotomy with floaters.
The circular pattern laser shots avoid the visual axis which resulted in decreased frequency of IOL Pitting which can cause glare and light scattering and be visually disabling. Thus, the circular technique can prevent any damage near the visual axis of IOL and generate sufficiently large size of the capsulotomy to restore contrast sensitivity and overcome glare disability. In patients who underwent circular pattern capsulotomy there was an immediate improvement of VA compared to these who underwent conventional cruciate method.
Mahmood Soni Wali et al study done on 58 patients were divided into two groups. In one group cruciate pattern of laser shots were given and in the 2nd group circular pattern of laser shots was used. Immediate visual outcome on 1st day was better with circular pattern. The incidence of IOP spike was less with circular pattern as compared to cruciate pattern. The IOL Lens pitting, CME and retinal detachment were not observed in patients who underwent circular pattern laser capsulotomies [6].
In our study in cases who underwent circular pattern complications like IOL pitting (83.3%), uveitis (75%) and CME (100%) are common compared cruciate pattern IOP spikes (55%) and Hyaloid face rupture (100%) is common in cruciate pattern compared to circular pattern.
The cruciate pattern Nd: YAG posterior laser capsulotomy can be performed safely but visual prognosis is better in circular pattern of capsulotomy. Complications like IOL pitting, uveitis and CME are common in cases who underwent circular pattern compared to cruciate pattern IOP spikes and Hyaloid face rupture is common in cruciate pattern.
- Steinberg EP, Javitt JC, Sharkey PD, Zuckerman A, Legro MW, et al. The content and cost of cataract surgery. Arch Ophthalmol. 1993; 111: 1041-1049. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8352686
- Sawusch MR, Guyton DL. Optimal astigmatism to enhance depth of focus after cataract surgery. Ophthalmology. 1991; 98: 1025-1029. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/1891208
- Gardner KM, Straatsma BR, Pettit TH. Neodymium: YAG laser posterior capsulotomy: the first 100 cases at UCLA. Ophthalmic Surg. 1985; 16: 24-28. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/3838376
- Aron-Rosa D, Aron JJ, Griesemann M, Thyzel R. Use of the neodymium-YAG laser to open the posterior capsule after lens implant surgery: a preliminary report. J Am Intraocul Implant Soc. 1980; 6: 352-354. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/7440377
- Kim Y, Park J. The effect of two different opening patterns of neodymium: YAG laser posterior capsulotomy on visual function. J Korean Ophthalmol Soc. 2012; 53: 390-395.
- Kara N, Evcimen Y, Kirik F, Agachan A, Yigit FU. Comparison of two laser capsulotomy techniques: cruciate versus circular. Semin Ophthalmol. 2014; 29: 151-155. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24475914