More Information
Submitted: 31 August 2020 | Approved: 28 September 2020 | Published: 29 September 2020
How to cite this article: Ademe S, Edmealem A. Pattern of ocular diseases among patients attending ophthalmic outpatient department: A cross-sectional study. Int J Clin Exp Ophthalmol. 2020; 4: 049-053.
DOI: 10.29328/journal.ijceo.1001033
Copyright Licence: © 2020 Ademe S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Pattern; Ocular disease; Morbidity; Borumeda Hospital; Ethiopia
Abbreviations: BMPH: Borumeda Primary Hospital; BRVO: Branch Retinal Vein Occlusion; CRVO: Central Retinal Vein Occlusion; D: Diopter; IAPB: International Agency for Prevention of Blindness; IOP: Intra Ocular Presses; MRN: Medical Registration Number; NLDO: Naso Lacrimal Duct Obstruction; OPD: Out Patient Department; SD: Standard Deviation; SPSS: Statistical Package of the Social Sciences; UCVA: Uncorrected Visual Acuity; VA: Visual Acuity
Pattern of ocular diseases among patients attending ophthalmic outpatient department: A cross-sectional study
Sewunet Ademe1* and Afework Edmealem2
1Wollo University, Department of Comprehensive Nursing, Ethiopia
2Department of Comprehensive Nursing, Ethiopia
*Address for Correspondence: Sewunet Ademe, Wollo University, College of Medicine and Health Sciences. Department of Comprehensive Nursing, Ethiopia, Tel: + 251918126233; Email: [email protected]
Background: Ocular diseases affect every individual in this world, with the only difference being in the pattern of occurrence of disease depending on age, gender, region, and climatic conditions. In Ethiopia there is shortage of literatures stating pattern of ocular diseases which is very important for planning preventive, curative and rehabilitative health service concerning prevalence of eye problems.
Objective: This study is aimed to determine the pattern of eye diseases at Borumeda Hospital, Amhara region, Ethiopia from July 10 to December 15, 2018.
Method: Institutional based cross- sectional retrospective study was conducted among 384 patients attending in ophthalmic OPD of Borumeda primary hospital. Nine hundred three newly diagnosed patients who were registered on OPD registration book in the study period were study population. Systematic random sampling was conducted to select study participants from study population. The collected data were then analyzed using descriptive statistics (mean and frequency percentage).
Results: From all study participants who had ocular disorders 92(24%) of them were came by Allergic conjunctivitis, followed by cataract 16.9%, refractory disorders 13%, Glaucoma 7.1%, infective conjunctivitis 4.7%, Pterygium 3.1%, Blepharitis 3.1%, NLDO 2.6%, Pseudoaphekia 2.4% and Corneal opacity 2.1%.
Conclusion: Significant number of patients 182(47.5%) of them came for treatment of adnexa (lid, margin, conjunctiva, lacrymal system) disorders. So every health professional should be responsible to deliver preventive, curative and rehabilitative services to control the most prevalent ocular disorders.
Significance of study: This study will be very important for health managers to distribute medical resources and staffs according to the prevalence of ocular disorders. This study result will be useful for health care workers for planning preventive, curative and rehabilitative health services for those common eye disorders.
Ocular diseases affect every individual in this world, with the only difference being in the pattern of occurrence of disease depending on age, gender, region, and climatic conditions. The majority of these ocular conditions which can lead to blindness are either potentially preventable or curable [1].
Disease pattern is in a state of constant flux, over a period of time. The pattern of eye diseases differs in developing and developed countries and often in communities [2]. The common ocular diseases worldwide are cataract, glaucoma, conjunctivitis, corneal ulcers, uveitis, refractive errors, and pterygium. From Benin City (Nigeria) reported that refractive errors, conjunctivitis, cataract, and glaucoma were reported to be the common eye diseases. In Sudan and other African countries, studies carried out on the pattern of ocular diseases in children have shown that refractive errors, allergic, and infective conjunctivitis are the most common causes of ocular morbidity [3-6].
Ethiopia was one of the highest blindness prevalence rates in the world, with 1.6 million blind people and an estimated 3.7 million people suffering from visual impairment. Although over 90% of blindness and visual impairment in the region is preventable [7]. The most common eye diseases seen among patients attending ophthalmic outreach services in a rural area in Ethiopia were conjunctivitis (29%), cataract (16.3), presbyopia (15.4%), refractive errors (7.9%), and blepharitis (7.5%) [7]. In general, the pattern of ocular diseases varies in different parts of the world and is influenced by racial, geographic, socioeconomic and cultural factors [6-10].
In Ethiopia particularly in the study region there is shortage of literatures stating pattern of ocular diseases which is very important for planning preventive, curative and rehabilitative health service concerning eye problems. The aim of this study is to determine the pattern of eye diseases at Borumeda Hospital Dessie town and it is hoped that this study will show the trend of ocular morbidities in our community and help to provide basic data for planning and provision of adequate eye care services, appropriate treatment, and intervention for those diseases. The study will also be used as baseline study for regional health policy makers and for those who need to conduct similar study in Ethiopia.
Study Design: Institutional based cross-sectional retrospective study deign was conducted.
Study Period: The study was conducted from July 10 to December 15, 2018.
Source Population: The source population were all patients who were registered on BMPH eye OPD registration book.
Study population: The study population was all newly diagnosed patients who were registered on BMPH eye OPD registration book from July 10 to December 15, 2018.
Sample size determination
The number of study participants that were recruited in to the research was calculated using the single Population proportion formula.
Sample size was calculated by considering level of confidence of 95%, and margin error 5% Where p - Proportion of patients (50%) who would have ocular disease q- Proportion of patients (50%) who didn’t have ocular diseases, d2-margin of error, N- minimum sample size. Substituting the values for each of these variables in the above formula,
Therefore the final sample size was = 384
Sampling technique and procedure
Systematic random sampling was conducted through calculating Kth value by dividing 903(sample frame) to 384(sample size) =2 then selected by lottery method for 1st 2 patients from documents so we take cases or patients for every other patient (cases). After that, we had taken the patient chart from the chart room and collected the data based on questionnaire adopted from different literatures by investigators.
Operational definition
Other adnexal diseases –relatively rare adnexal diseases those were not included in the check list of our study like pingueclua, conjunctival nevus, squamous cell carcinoma, dry eye, preseptal cellulitis etc...
Other anterior segment diseases –diseases of anterior segment of the eye those who were not included in the check list of our study like corneal staphyloma, band keratopathy, spheroidal degeneration etc...
Other posterior segment diseases–diseases of posterior segment of the eye those were not included in the check list of our study like macular scar, macular hole, optic atrophy etc...
Others- ocular problems those can’t be specified in adnexa, anterior segment or posterior segment of the eye like refractive error, strabismus, endophthalmitis etc…
Ensuring data quality
Every patient visual acuity (VA) and IOP were first measured by trained health workers then, patients were examined by optometrist, ophthalmic nurses or cataract Surgeons and the patients who need senior examination were examined by ophthalmologist by using slit lamp, direct ophthalmoscope or 90D lens as needed. The data was collected by well oriented ophthalmic nurses after we had tested the checklist and the diagnosis was selected based on the most senior diagnosis of patient chart.
Data Processing and Analysis: Data was entered and analyzed using the Statistical Package of the Social Sciences (SPSS) software and presented as simple frequencies, pie-chart cross-tabulations or bar graph.
Ethical Consideration: The ethical issue of this study was approved by the ethical committee of the college of Medicine and Health science. We had communicated with Borumeda primary hospital about the study through letter written by Wollo University, and official permission was taken from the BMPH office to conduct the study.
Out of the total three hundred eighty four ocular patients 197(51.3 %) of them were females and 186(48.4%) were males. From all 72(18.8%) of them were within age 21-30 years, out of all 61(15.9%) of them were within the age of 31-40 years 56(14.6%) of them were within the age of 51-60 years. From all study subjects who came to Borumeda hospital for treatment of ocular disorders 381(99.2%) of them came from the Amhara region (Table 1).
| Table 1: Socio-demographic characteristics among study participants in Borumeda hospital Eye OPD, December, 2018. (n = 384). | |||
| Variables | Category | Frequency | Percent |
| Sex | Female | 197 | 51.4 |
| Male | 186 | 48.6 | |
| Age | 1-10 | 31 | 8 |
| 11-20 | 44 | 11.5 | |
| 21-30 | 72 | 18.75 | |
| 31-40 | 61 | 15.9 | |
| 41-50 | 55 | 14.3 | |
| 51-60 | 56 | 14.6 | |
| 61-70 | 41 | 10.7 | |
| 71-80 | 17 | 4.4 | |
| >80 | 3 | 0.8 | |
| Region | Amhara | 381 | 99.2 |
| Others | 3 | 0.8 | |
| Zone | South Wollo | 311 | 81 |
| Other zones | 73 | 19 | |
Pattern of ocular disease
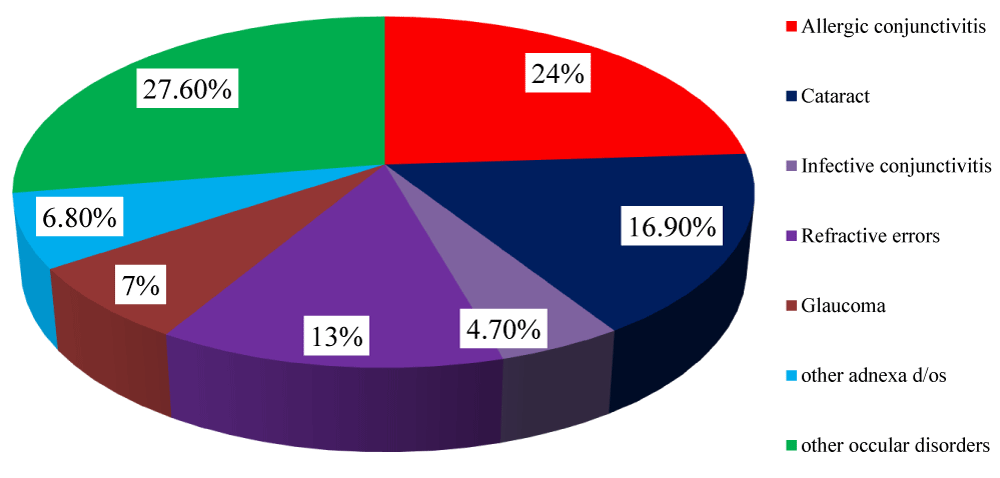
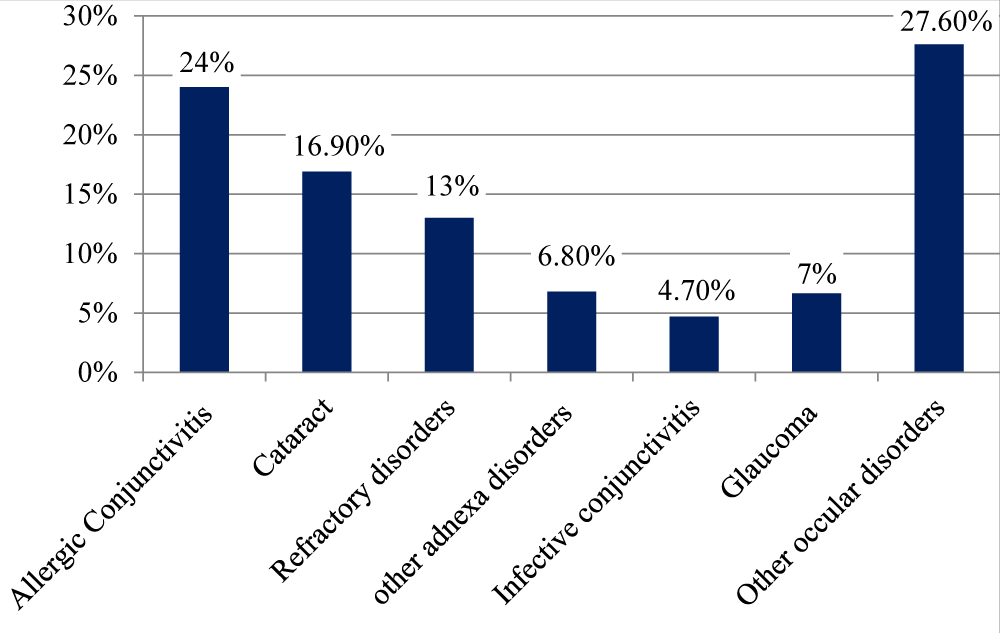
The findings of this study had shown that out of all 384 study participants, 182(47.5%) of patients came for treatment of adnexa (lid, margin, conjunctiva, lacrymal system) disorders, Among this adnexa disorders; from all study participants 92(24%) of them were came by Allergic conjunctivitis patients, 18(4.7%) of them came by infective conjunctivitis,12(3.1%) of them came by blepharitis, 26(6.8%) of them came by adnexa disorders of eye, the findings of this study had shown that among 384 study participants 118(30.7%) of them came to Borumeda hospital by anterior segment(cornea, sclera, Iris, pupil, AC, lens)disorder. Among this anterior segment disorders 65(16.9%) of them came by cataract, of them 9(2.4%) of respondents came by uveitis, 9(2.4%) of them by pseudoaphekia, 8(2.1%) of them by corneal opacities and 21(5.5%) of them came by other anterior segment disorders. Among all study participants 82(21.4) of them came to Borumeda hospital by other posterior segment disorders, among this 50(13%) of them were come by refractive errors, 27(7.1) of them came by glaucoma (Table 2) (Figures 1,2).
| Table 2: Pattern of ocular disease among study participants in Borumeda hospital Eye OPD, December, 2018 [n=384]. | ||||
| Variables | Class of disease | Frequency | Percent | |
| T. Trichiasis Entropion |
Adnexa disorders | 10 | 2.6 | |
| Adnexa disorders | 1 | 0.3 | ||
| NLDO Allergic conjunctivitis Infective conjunctivitis |
Adnexa disorders | 10 | 2.6 | |
| Adnexa disorders | 92 | 24 | ||
| Adnexa disorders | 18 | 4.7 | ||
| Pterygium | adnexa disorders | 12 | 3.1 | |
| Chalazion | adnexa disorders | 1 | 0.3 | |
| Blepharitis | adnexa disorders | 12 | 3.1 | |
| Other adnexal disorders | 26 | 6.8 | ||
| Cornial opacity | Anterior segment disorders | 8 | 2.1 | |
| Keratitis | Anterior segment disorders | 6 | 1.6 | |
| Uveitis Cataract |
Anterior segment disorders | 9 | 2.4 | |
| Anterior segment disorders | 65 | 16.9 | ||
| Pseudoaphekia | Anterior segment disorders | 9 | 2.4 | |
Other anterior disorders
Retinal detachment |
posterior segment disorders posterior segment disorders posterior segment disorders |
21 27 2 2 |
5.5 7.1 0.6 0.6 |
|
| Diabetic retinopathy | Posterior segment disorders | 0.3 | ||
| Other posterior disorders | 2 | 0.5 | ||
| Refractive Error | Other posterior segment disorders | 50 | 13 | |
Figure 1: The pattern of ocular disease among patients in Borumeda hospital Eye OPD clinic, December, 2018, Dessie, Ethiopia (n = 384).
Figure 2: The pattern of ocular disease among patients in Borumeda hospital Eye OPD clinic, December, 2018, Dessie, Ethiopia (n = 384).
From the total of 384 study participant’s 92(24%) of them had Allergic conjunctivitis, out of this 65(16.9%) of them had Cataract and 50(13%) of them had refractory disorders.
Data coming from this study ascertained that 197(51.3%) of them were females and 186(48.4%) were males, but the study conducted in western Nepal had shown that from total of 915 patients out of which 617(67.5%) were females and 298(32.5 %) were males, study conducted in India had shown that 47.3% were males and 52.7% were female and in Nigeria 56% of study participants were females and 44% of them were males. In other study conducted on ocular morbidity of patients attending ophthalmic outreach services in rural Ethiopia by the year 2013, indicated that, a total of 214 patients were examined, where males comprised of 50.5% [7,11,13,14]. This might be due to difference in sample size and gender pattern of countries.
From all study participants 72(18.8%) of them were within age 21-30 years, out of all 61(15.9%) of them were within the age of 31-40 years 56(14.6%) of them were within the age of 51-60 years. Out of the total study participants 311(81%) of them were came from south Wollo zone and the remaining 19% of them were came from other zones. From all study subjects who came to Borumeda hospital for treatment of ocular disorders 381 (99.2%) of them came from the Amhara region. Out of all study participants 99(25.8%) of them were came from Dessie.
The findings of this study had shown that out of all study participants, 182(47.5%) of patients came for treatment of adnexa (lid, margin, conjunctiva, lacrymal system) disorders, Among this adnexa disorders from all study participants 92(24%) of them were came by Allergic conjunctivitis, followed by cataract 16.9%, refractive errors 13%, glaucoma 7.1%, infective conjunctivitis 4.7%, Pterygium 3.1%, Blepharitis 3.1%, NLDO 2.6%, Pseudoaphekia 2.4%, Cornial opacity 2.1%.
But the study conducted in western Nepal had shown that refractive error was the most common ocular morbidity accounting 26.8% followed by conjunctivitis20.6%, cataract 11.8%, pterygium 6%, chalazion/sty 4%, ectropion/entropion 3.9%, keratitis 3.8%, dry eyes 2.8%, and corneal opacities 2.3% [11].
The study conducted in pakistan had shown that patients who presented with infectious conjunctivitis (mostly trachoma) (24%) and with cataract (23.1%), followed by those who presented with refractive error (17.4%). Presentation of pterygium and corneal ulcer was 11.0% and 3.02% respectively. Cases of glaucoma and strabismus were 2.8% and 1.28% respectively [13]. The study conducted in Nigeria, indicated that, the common ocular conditions seen were presbyopia (28.3%), allergic conjunctivitis (22.6%), pingueculae (18.0%), ocular hypertension (8.8%), pterygium (8.3%), cataract (7.8%), and uncorrected refractive error (6.0%) [15]. Study conducted in Sudan had shown that the most common eye disorder encountered was cataract (26.66%); this was followed by allergic conjunctivitis (23.77%) and infective conjunctivitis (23.35%). Refractive errors (16.42%) and presbyopia (11.29%). In other study conducted on ocular morbidity of patients attending ophthalmic outreach services in rural Ethiopia by the year 2013, indicated that, a total of 214 patients were examined, where males comprised of 50.5%. Ocular diseases were quite prevalent among the study group. Conjunctivitis was the primary ocular morbidity accounting for 29%, followed by cataract (16.3%), presbyopia (15.4%), refractive errors (7.9%), Blepharitis (7.5%) [6,13,15].
This might be due to difference in sample size, place study conducted, socio-economic status of the population and health service of the country like mass treatment of population, screening service for each ocular diseases and decentralized timely treatment.
In this study we are facing difficulties of getting some of the socio-demographic characteristics, Limitation of related literatures to compare and discuss some of the findings and because the data are cross sectional, the direction of causal relationship between variables can’t always be determining.
The findings of this study revealed that Allergic conjunctivitis, cataract, refractory disorders, glaucoma, and infective conjunctivitis were the most prevalent ocular disorders in the area so regional health officials and all clinicians should target to solve this problems by extending the health care service to rural areas.
This article was sponsored by the deputy of research and technology of Wollo University college of Medicine and health sciences. The authors would like to appreciate the Clinical Research of Wollo University College of medicine and health science as well as Borumeda general hospital staffs and officials of the hospital who helped us in this research.
Funding: The study was funded by Wollo University.
Availability of data and materials: Data are available by contacting the corresponding author.
Authors ‘contributions: SA and AE contributed to designing the study, SA collected the data, SA analyzed the data and AE and wrote the final report and manuscript. All the authors read and approved the version for submission.
Ethics approval and consent to participate: Ethical approval was obtained from the Ethical Review Committee of Wollo University. Written informed consent was obtained from all participants.
Consent for publication: All the participants consented to publish the study in this journal.
- Murad MAU. Pattern of eye diseases in a tertiary hospital in Suburban area. Nepal. The origin MJ. 2007; 28꞉ 492- 494.
- Agyemang Mireku. Pattern of ocular conditions among patients attending an eye clinic in Ghana. Optom open access. 2017; 2꞉ 2476- 2075.
- Mehari ZM. Pattern of childhood ocular morbidity in rural eye hospital. Central Ethiopia. BMC ophthalmology. 2014; 14: 1471- 2415. PubMed: https://pubmed.ncbi.nlm.nih.gov/24731554/
- Workoma FS, Ichenwo T. Pattern of eye disorders in Ogbodo: A rural community in rivers state, Nigeria. The Nigerian HJ. 2011; 11: 14-18.
- Rizyal. A study of ocular morbidityof patients attending a satellite clinic in Bhaktapur, Nepal. Nepal med col J. 2010; 12: 87-89. PubMed: https://pubmed.ncbi.nlm.nih.gov/21222404/
- Khalil AL, Atif B Mohamed Ali. Pattern of eye diseases at Makah tertiary eye hospital, Khartoum, Sudan. 2015; 3: 15-18.
- Zelalem A. A study of ocular morbidity of patients attending ophthalmic outreach services in rural Ethiopia. Int J Med. 2013; 3: 450- 454.
- Oluwatoyi O, Adenike A. Childhood eye diseases in south western Nigeria: A tertiary hospital study. Clinic J. 2009; 64: 947-951. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2763068/
- Rajani G, Arun G. A cross-sectional study to assess the morbidity pattern of ocular diseases in out-patient department of ophthalmology at Bhilwara, Rajasthan, India. Indian J. 2016; 6: 800-803.
- Joseph ML. Pattern of ocular findings among patients aged 40 years and above attending eye clinic at Juba teaching hospital, southern Sudan. Unpublished. 2014.
- Sarita T, Sachin D. Pattern of ocular morbidity in patients attending an ophthalmic in a rural part of western Nepal. Nobel MCJ. 2011; 2: 27-30.
- Ramesh RB, Sagar R, Anu G, Pratik C. Profile of ophthalmological diseases in out-patients of Shree Birendra hospital, Kathmandu, Nepal. MJSBH. 2013; 12: 5-11.
- Uzma F, Arshad S, Atiya R, Fehmi MS, Rais M. Review of out-patient department Spencer eye hospital, Pakistan. Pak J. ophthalmology. 2013; 29: 16-20.
- Shubhra M, Manbir S. Pattern of ocular diseases in children attending outpatient department of a rural medical college in central India. Int. JSS. 2015; 3: 57-60.
- Bola J Adekoya, et al. Pattern of eye diseases among commercial intercity vehicle drivers in Nigeria. Nig J. 2008; 16: 55-59.
- Ajaiyeoba AI1, Isawumi MA, Adeoye AO, Oluleye TS. Pattern of eye diseases in south western Nigeria. Int Ophthamol. 2007; 27: 287-292.
- Oladigbolu KK, et al. Pattern of eye diseases in a university health service clinic in northern Nigeria. Nig JM. 2012; 21: 334-337. PubMed: https://pubmed.ncbi.nlm.nih.gov/23304932/