More Information
Submitted: September 30, 2021 | Approved: October 08, 2021 | Published: October 11, 2021
How to cite this article: Chaimae K, Ahmed B, Fouad C, Meriem A, Idriss BA. Bilateral corneal ulcer and hypovitaminosis A: a case report. Int J Clin Exp Ophthalmol. 2021; 5: 023-024.
DOI: 10.29328/journal.ijceo.1001039
Copyright Licence: © 2021 Chaimae K, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Progressive supranuclear palsy; Parkinson’s disease; Diplopia; Vertical gaze palsy; Multisystem atrophy
Bilateral corneal ulcer and hypovitaminosis A: a case report
Khodriss Chaimae1*, Bennis Ahmed2, Chraibi Fouad2, Abdellaoui Meriem3 and Benatiya Andaloussi Idriss3
1MD, Ophthalmology Department, Hassan II Hospital, Sidi Mohammed Ben Abdellah University, Fez, Morocco
2MD, Assistant Professor, Ophthalmology Department, Hassan II Hospital, Sidi Mohammed Ben Abdellah University, Fez, Morocco
3MD, Professor, Ophthalmology Department, Hassan II Hospital, Sidi Mohammed Ben Abdellah University, Fez, Morocco
*Address for Correspondence: Khodriss Chaimae, MD, Ophthalmology Department, Hassan II Hospital, Sidi Mohammed Ben Abdellah University, Fez, Morocco, Email: [email protected]
Vitamin A is a fat-soluble discovered in 1913. Hypo-vitaminosis A can cause blindness by various mechanisms. The aim of this case report is to emphasize the severity of Vitamin A deficiency and its local consequences on the eyes causing corneal ulcerations, abscess and even blindness.
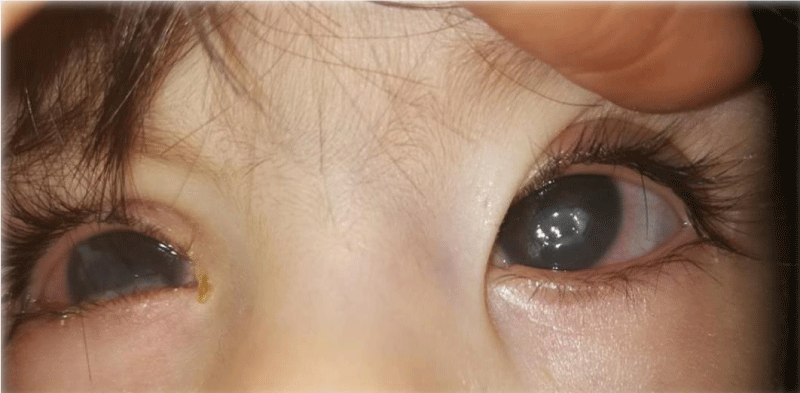
A 10-month-old baby with a history of psychomotor and staturoponderal delay was referred to our department for a red eye and photophobia. The clinical examination showed a positive glare reflex but the child was unable to catch the objects. The patient had mucopurulent discharge of both eyes, conjunctival hyperemia, and total bilateral corneal ulcer with an axial bilateral corneal abscess (Figure 1) without visible hypopyon in the anterior chamber. The ultrasound screen of the eye was normal.
Figure 1: Image showing the bilateral abscess of the patient.
Microbiological analysis reveal gram + cocci. The biological tests showed collapsed levels of serum retinol which is an important indicator of Vitamin A status.
The patient received treatment with topic antibiotic therapy (ciprofloxacin, tobramycin), artificial tears and topic vitamin A. Few day after the treatment the corneal ulcer was completely healed and a corneal opacity with neovascularization took place (Figure 2).
Figure 2: Image showing the final appearance of the cornea after stopping treatment.
Hypovitaminosis A was endemic in most countries in the world, and it has been the most important cause of childhood blindness in developing countries.
This deficiency is usually due to malnutrition, digestive malabsorption secondary to celiac disease or to bariatric surgery to treat severe obesity, it causes approximately 250,000 cases of blindness each year [1].
Vitamin A deficiency and xerophthalmia affect an estimated 750 million people worldwide [2]. Xerosis and keratinization of focal areas of the cornea were experimentally shown to be associated with corneal ulcers and a rapidly developing keratomalacia [2].
Because of its origin, xerophthalmia is found in chronic diseases of the intestine with malabsorption, liver, and pancreas disease, chronic infectious disease, iron-deficiency anemia, and in cases of increased metabolic rate, such as hyperthyroidism [3]. Vitamin deficiency occurring in newborns and resulting in ocular defects appears to be quite rare. Except for vitamin A deficiency, no reports were found of ocular defect occurring as a result of neonatal deficiencies in vitamins D or K or iron. Intrinsic disorders of vitamin A metabolism can also produce a variety of ocular malformations in children [4]. Vitamin A plays a crucial role in ocular embryogenesis and retinal function; therefore its deficiency has provided insight into the molecular roles of vitamin A in the appearance of the malformations identified in murine models and in human patients [5]. Two biochemical indicators are currently used to determine vitamin A deficiency: serum retinol and serum RBP. A cutoff for serum retinol concentration has been proposed at less than 0.70 μmol/L [6].
In developed countries, the cause is mostly due to malabsorption. This malabsorption of vitamin A can be caused by structural or functional abnormality of the gastrointestinal system. Previous cases of vitamin A deficiency in the developed world have been reported after cystic fibrosis [7] primary biliary cirrhosis [8], jejunoileal bypass surgery [9], hemicolectomy [10] and bariatric surgery [11]. Selective dietary restrictions leading to hypovitaminosis A can also be influenced by behavioural challenges in food faddism, psychoses, as well as neurodevelopmental [1,12] and psychiatric disorders [13].
Of all the micronutrient deficiencies, that of vitamin A has had both the most intensive investigation and the most aggressive investment. The role of periodic high dose supplementation as a measure against child mortality but not as a mean to sustain an adequate vitamin status.
Because vitamin A deficiency is prevalent among population below the extreme poverty line, the most needy are often not reached by the attempts to reduce the deficiency. Biofortification of plant sources shows a lot of promise to improve sustainability the fortification form that does not risk excessive superimposition of sources of provitamin A [14].
Authors’ contributions
All the authors contribute to the management of this case and the redaction of this manuscript. All the authors have given their approval to the final version of the manuscript.
- Collins CE, Koay P. Xerophthalmia because of dietary-induced vitamin a deficiency in a young Scottish man. Cornea. 2010; 29: 828‑829. PubMed: https://pubmed.ncbi.nlm.nih.gov/20489600/
- Lee WB, Hamilton SM, Harris JP, Schwab IR. Ocular Complications of Hypovitaminosis A after Bariatric Surgery. Ophthalmology. 2005; 112: 1031‑1034. PubMed: https://pubmed.ncbi.nlm.nih.gov/15885783/
- Panozzo G, Babighian S, Bonora A. Association of xerophthalmia, flecked retina, and pseudotumor cerebri caused by hypovitaminosis A. Am J Ophthalmol. 1998; 125: 708‑710. PubMed: https://pubmed.ncbi.nlm.nih.gov/9625560/
- Underwood BA. Maternal vitamin A status and its importance in infancy and early childhood. Am J Clin Nutr. 1994; 59: 517S-522S. PubMed: https://pubmed.ncbi.nlm.nih.gov/8304290/
- Niederreither K, Dollé P. Retinoic acid in development: towards an integrated view. Nat Rev Genet. 2008; 9: 541‑553. PubMed: https://pubmed.ncbi.nlm.nih.gov/18542081/
- Pee S de, Dary O. Biochemical indicators of vitamin A deficiency: Serum retinol and serum retinol binding protein. J Nutrit. 2002; 132: 2895S-2901S. PubMed: https://pubmed.ncbi.nlm.nih.gov/12221267/
- Rayner RJ, Tyrrell JC, Hiller EJ, Marenah C, Neugebauer MA, et al. Night blindness and conjunctival xerosis caused by vitamin A deficiency in patients with cystic fibrosis. Arch Dis Child. 1989; 64: 1151-1156. PubMed: https://pubmed.ncbi.nlm.nih.gov/2789497/
- Walt RP, Kemp CM, Lyness L, Bird AC, Sherlock S. Vitamin A treatment for night blindness in primary biliary cirrhosis. Br Med J (Clin Res Ed). 1984; 288: 1030‑1031. PubMed: https://pubmed.ncbi.nlm.nih.gov/6423181/
- Tripathi RC, Tripathi BJ, Raja SC, Partamian LS. Iatrogenic ocular complications in patients after jejunoileal bypass surgery. Int Surg. 1993; 78: 68‑72. PubMed: https://pubmed.ncbi.nlm.nih.gov/8473089/
- Sloan DB, Wood WJ, Isernhagen RD, Schmeisser ET. Short-term night blindness associated with colon resection and hypovitaminosis A. Arch Ophthalmol. 1994; 112: 162‑163. PubMed: https://pubmed.ncbi.nlm.nih.gov/8311764/
- Fok JS, Li JYZ, Yong TY. Visual deterioration caused by vitamin A deficiency in patients after bariatric surgery. Eat Weight Disord. 2012; 17: e144-146. PubMed: https://pubmed.ncbi.nlm.nih.gov/23010786/
- Cornea, 2-Volume Set - 4th Edition 2021. https://www.elsevier.com/books/cornea-2-volume-set/mannis/978-0-323-35757-9
- Cooney TM, Johnson CS, Elner VM. Keratomalacia caused by psychiatric-induced dietary restrictions. Cornea. 2007; 26: 995‑997. PubMed: https://pubmed.ncbi.nlm.nih.gov/17721303/
- Solomons NW. Plant sources of vitamin A and human nutrition: red palm oil does the job. Nutr Rev. 1998; 56: 309‑311. PubMed: https://pubmed.ncbi.nlm.nih.gov/9810811/