More Information
Submitted: March 01, 2022 | Approved: April 23, 2022 | Published: April 24, 2022
How to cite this article: Kaushal H, Sulena. Chlorambucil induced papilledema: a serious yet reversible side effect of chemotherapy. Int J Clin Exp Ophthalmol. 2022; 6: 013-014.
DOI: 10.29328/journal.ijceo.1001044
Copyright Licence: © 2022 Kaushal H, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Chlorambucil induced papilledema: a serious yet reversible side effect of chemotherapy
Himanshu Kaushal1* and Sulena2
and Sulena2
1Senior Resident, Department of Medicine, Guru Gobind Singh Medical College and Hospital, Faridkot, Punjab, India
2Associate Professor, Division of Neurology, Guru Gobind Singh Medical College and Hospital, Faridkot, Punjab, India
*Address for Correspondence: Dr. Himanshu Kaushal, Senior Resident, Department of Medicine, Guru Gobind Singh Medical College and Hospital, Faridkot, Punjab-151203, India, Email: [email protected]
Papilledema is optic disc swelling due to high intracranial pressure. Possible conditions causing high intracranial pressure and papilledema include intracerebral mass lesions, cerebral hemorrhage, head trauma, meningitis, hydroce-phalus, spinal cord lesions, impairment of cerebral sinus drainage, anomalies of the cranium, and idiopathic intracranial hypertension (IIH) [1].
Chlorambucil is an antineoplastic in the class of alkylating agents that is used to treat various forms of cancer [2].
A 45-year-old male known case of chronic lymphocytic leukemia (CLL) on chemotherapy (chlorambucil) presented with the bilateral blurring of vision that was insidious in onset and gradually progressive for the last 20 days. No history of pain on eyeball movements. No history of trauma. No history of fever.
The patient had a history of headaches. No history of vomiting. No history of weakness of any part of the body.
Nonhypertensive, nondiabetic, nonalcoholic, nonsmoker.
On Examination:
Higher mental function: Normal; Speech, Language, Memory: Normal.
Cranial nerve examination:
Cranial nerve II: Visual Acuity CF 0.5m in the right eye, 6/12 in the left eye.
Cranial nerve VIII: Bilateral Moderate SNHL.
Rest cranial nerves: Normal; Tone, Power, Reflexes: Normal.
Sensory examination and cerebellar signs: Normal.
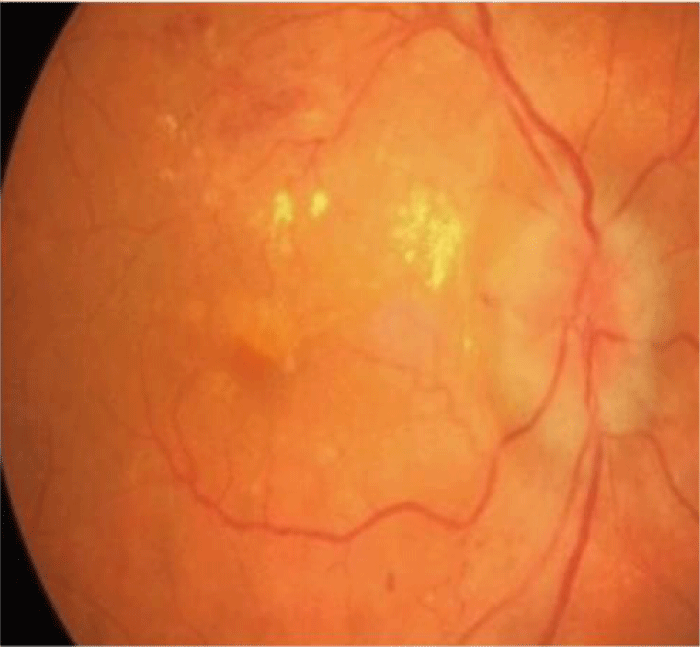
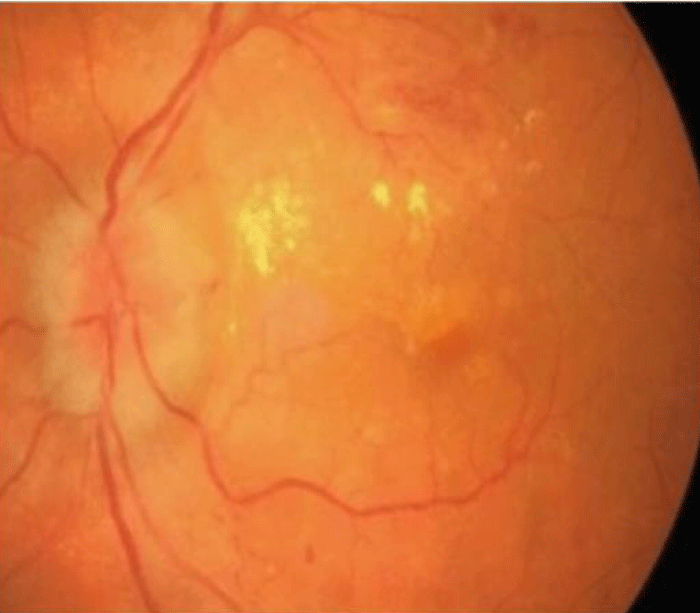
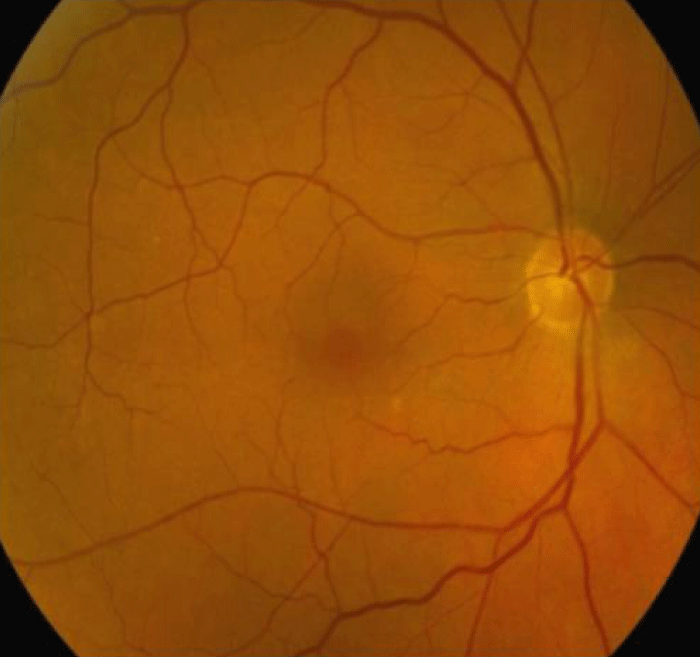
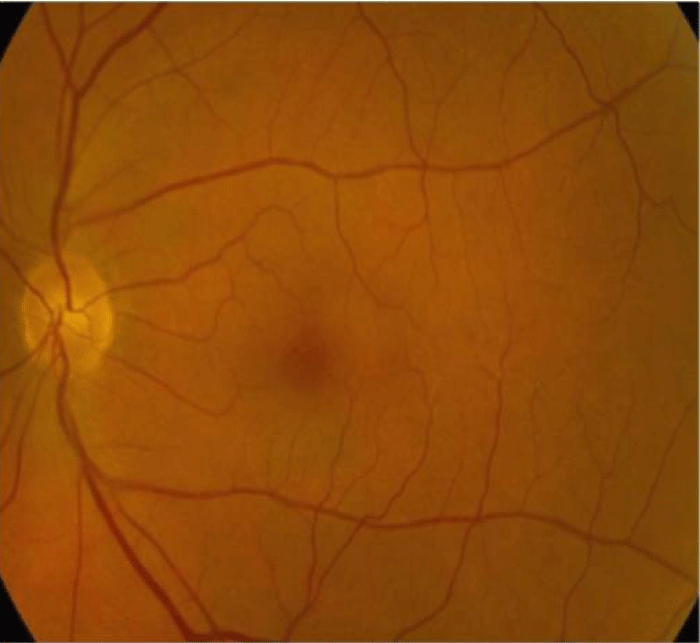
The patient was started on antiedema measures in the form of acetazolamide, methylprednisolone pulse therapy 500 mg for 5 days, and chlorambucil was stopped temporarily after consultation with the oncologist. The patient had improvement in vision (Figures 1-4). Post-treatment Visual Acuity: 6/6 in both eyes.
MRI Brain with orbit: Bilateral optic neuritis.
Figure 1: Shows bilateral optic disc edema before starting the antiedema measures.
Figure 2: Shows bilateral optic disc edema before starting the antiedema measures.
Figure 3: howing resolved bilateral optic disc edema.
Figure 4: Showing resolved bilateral optic disc edema.
Ocular toxicity induced by cancer chemotherapy is not uncommon, but the broad spectrum of reactions to injury displayed by the eye reflects the unique anatomical, physiological, and biochemical features of this essential organ. Several cases of keratitis and a single case of diplopia with bilateral papilledema and retinal hemorrhages have been reported as ocular side effects of chlorambucil [3]. CLL itself can infiltrate the eye and optic nerve causing optic neuritis and papilledema however cytotoxic drug therapy is more common to cause toxic optic neuritis and papilledema. The mechanism behind this is poorly understood however the drug is directly toxic to the neurons of the optic nerve. It is long-term exposure to a drug that causes cumulative inflammatory damage to the optic nerve [4,5].
Chemotherapy drugs should be used with caution as drugs like chlorambucil can cause optic disc edema and other ocular toxicities. The patient should be kept on regular follow-up with an ophthalmologist for assessment of vision and disc status once the patient is on chemotherapy especially with drugs like chlorambucil.
- Rigi M, Almarzouqi SJ, Morgan ML, Lee AG. Papilledema: epidemiology, etiology, and clinical management. Eye Brain. 2015; 7: 47-57. PubMed: https://pubmed.ncbi.nlm.nih.gov/28539794/
- National Center for Biotechnology Information. "PubChem Compound Summary for CID 2708, Chlorambucil" PubChem. 2021. https://pubchem.ncbi.nlm.nih.gov/compound/Chlorambucil
- Bregeat M, Hernians R. Oedenia papillaire spontanerrient criable aucous d'um traitement par le chlorambucil. Bull SOC Beige Oplztlialmol. 1972; 1960567-69.
- Al-Tweigeri T, Nabholtz JM, Mackey JR. Ocular toxicity and cancer chemotherapy: A review. Cancer. 1996; 78: 1359-1373. PubMed: https://pubmed.ncbi.nlm.nih.gov/8839540/
- Gonsalves WI, Zent CS, Pulido JS, Patnaik MM. Visual loss in early-stage chronic lymphocytic leukemia. J Clin Oncol. 2013; 31: e280-e282. PubMed: https://pubmed.ncbi.nlm.nih.gov/23650405/