More Information
Submitted: March 09, 2022 | Approved: May 05, 2022 | Published: May 06, 2022
How to cite this article: Shah Z, Hussain I, Jan S, Mahar PS, Ishaq M, et al. Treatment of advance keratoconus using donor bowman layer: the zaman technique of bowman layer transplantation (Type I & Type II). Int J Clin Exp Ophthalmol. 2022; 6: 015-025.
DOI: 10.29328/journal.ijceo.1001045
Copyright Licence: © 2022 Shah Z, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Bowman layer (BL); Bowman layer transplantation(BLT); Penetrating Keratoplasty (PKP); Deep Anterior Lamellar Keratoplasty (DALK); Balance Salt Solution(BSS); Intra Corneal Ring Segment (ICRS)
Treatment of advance keratoconus using donor bowman layer: the zaman technique of bowman layer transplantation (Type I & Type II)
Zaman Shah1*, Ibrar Hussain1, Sanaullah Jan1, P S Mahar2, Mazhar Ishaq2 and Fawad Rizvi1
1Department of Ophthalmology, Khyber Teaching Hospital, Peshawar, Pakistan
2Department of Ophthalmology, Health Net Hospital, Peshawar, Pakistan
*Address for Correspondence: Zaman Shah, (MBBS, FCPS), Department of Ophthalmology, Khyber Teaching Hospital, Peshawar, Pakistan, Email: [email protected]
Commonly referred to as an ecstatic, non-inflammatory disease, Keratoconus, usually bilateral and asymmetric, is characterized by progressive steeping and thinning of the cornea. This results in irregular astigmatism which compromises vision [1,2]. Traditionally, early Keratoconus stages have been treated by prescribing a hard contact lens to obtain a regular anterior optical surface. This tendency was discontinued when contact lens intolerance in advanced stages required the use of penetrating keratoplasty (PKP) or deep anterior lamellar Keratoplasty (DALK). An alternative technique of corneal cross-linking was designed in 2003 as a treatment option for keratoconus. The cornea measured at least 400 um thickness after epithelium removal and pre-operative maximum keratometry (Kmax) measured 58D or less. As a result, no corneal transplantation was required or postponed [3].
In cases of advanced keratoconus, intrastromal corneal ring segment (ICRS) and UV cross-linking may not be an option because of insufficient corneal thickness. The corneal thickness of at least 400 um, and steeper cornea (Kmax more than 58D) [4,5] is the required thickness level for ICRS and UV cross-linking.
Complications like irregular astigmatism, suture-related problems, and severe ocular surface disease after performing PKP/DALK have been widely reported in scientific journals [6-8]. Performing this kind of surgery in eyes with significant peripheral thinning usually leads to an important and progressive astigmatic defect which may result in allograft rejection, cataract, and glaucoma [9,10].
Visual outcomes in eyes that have undergone Keratoplasty may be affected by several factors related to the ocular surface and anterior segments. These include tear film dynamics, anterior and posterior higher-order aberrations (HOAs), and corneal light scattering [15]. Considering the results of previous studies, which analyzed the amount of scattering produced by different lamellar keratoplasties, the bowman layer transplantation into the mid corneal stroma, may increase, as expected, some corneal backscattering [16]. After bowman layer transplantation the flattening effect of BL directly affects the spherical aberration.
Electron microscopy has revealed the breakdown and fragmentation as well as thinning of the bowman layer in advance keratoconus [11].
To strengthen the weak cornea of advanced keratoconus, a surgical technique, employing mid stromal BL transplantation, was developed to flatten and strengthen the weak cornea of advanced keratoconus [12]. This stipulated that long-term stabilization of keratoconus may be obtained by BL itself or the wound healing effect between the host stroma and BL graft [13,14].
The Zaman Technique of bowman layer transplantation type 1 & 11 is a new technique designed for the lamellar corneal transplantation procedures using either fibrin glue or a femtosecond laser. It is carried out for all those patients with advanced keratoconus who are otherwise ineligible for ultraviolet corneal cross-linkage or intrastromal corneal ring segments. It suggests deep anterior lamellar keratoplasty where there was none planned. This technique can also be performed at any age level and irrespective of the severity of vernal keratoconjunctivitis.
owman layer harvesting technique
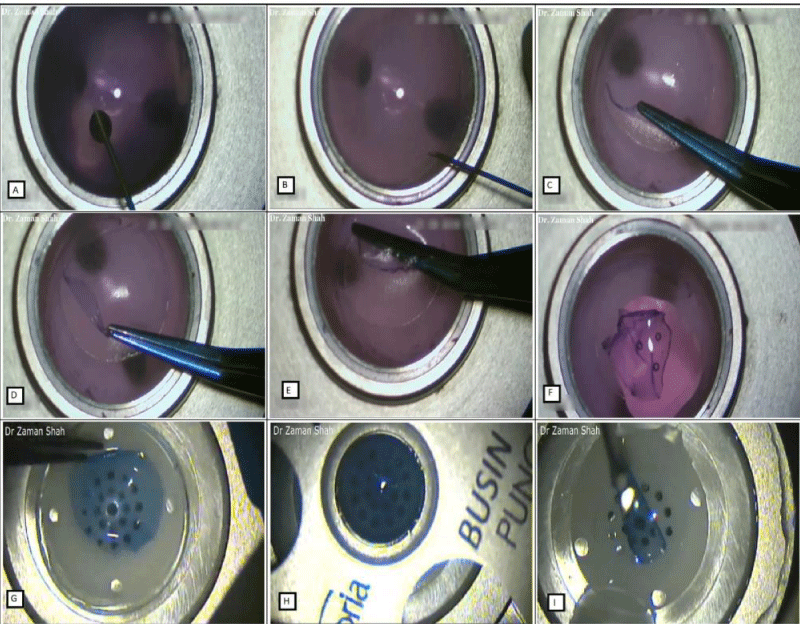
In Bowman Layer Harvesting Technique, a donor cornea with a scleral rim is mounted on an artificial anterior chamber using air. The epithelium is carefully removed by mechanical scraping with microsponge and SPATULA DOUBLE FLAP BURATTO Millennium Number: 87-6871. Vision blue is used to stain the bare Descemet membrane and at the same time air is injected into the stroma of the donor cornea for good visibility and easy peeling of the bowman layer. With a 30-gauge needle, a superficial incision is given at the corneal periphery inside the limbus over 3600 around, not so deep as to involve the corneal stroma as it will inadvertently increase the thickness of the bowman layer, which will make peeling difficult, and adherent residual keratocytes. The depth of the incision, the bowman layers harvesting technique stipulates, should be judged under the microscope showing only the marking. The bowman layer is carefully dissected from the corneal stroma, from the periphery to the center. During the process of harvesting, the bowman layer should not be kept completely wet or completely dry. Once the bowman layer is peeled off completely, it is sponged out on a contact lens, forming a membranous flap of 9.0 to 11.00 mm in diameter which spontaneously forms a roll due to its elastic properties (Figure 1g,h,i). The bowman layer is soaked in 70% ethanol to remove any remnants of epithelial cells and other keratocytes. After irrigation with balanced salt solution (BSS) it is stored in organ culture media at 300 for 6 weeks [17-19].
Figure 1: Intraoperative video frame of isolated bowman layer harvesting.
Surgical Technique for Bowman Layer Transplantation (An old technique, mentioned just for reference and comparison with the Zaman technique of BLT type 1 & 11).
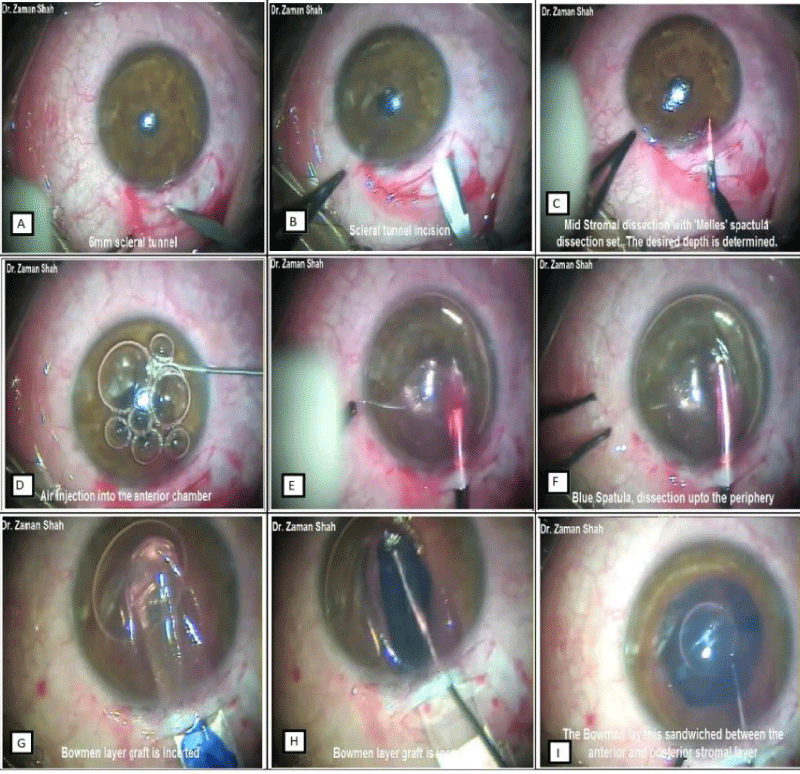
A 6 mm scleral tunnel is created 2 mm away from the limbus and manual mid stromal dissection is performed using deep dissecting Melle’s spatulas while the anterior chamber is filled with air. During dissections of the stroma, the black shadow surrounding the spatula is used as an indication for aimed dissections depth until a pocket is created from limbus to limbus 3600 around (Figure 2) using a red, blue, and white spatula. A Visitec surgical glide is inserted into the mid stromal pocket, while a larger part of the air bubble is removed from the anterior chamber. The bowman membrane is soaked in 70% ethanol to remove surface keratocytes and then thoroughly rinsed with balanced salt solution (BSS) and finally stained with vision blue. The bowman membrane is placed on the top of the glide with rolled margin facing down and inserted into the stromal pocket which is then unfolded and centered, using a bent 30G cannula and balance salt solution to manipulate the graft. The anterior chamber is filled with balance salt solution to maintain the normal intraocular pressure. No sutures are required to close the main incision or to fixate the graft, only the conjunctival wound is closed with cauterization.
Figure 2: Intraoperative video frame of the old technique of Bowman layer transplantation.
After mounting the donor button on the artificial anterior chamber stain with vision blue (A), 30 gauge needle is used to mark the boundaries of bowman layer 3600 around after removal of the epithelium with microsponges (B), MC Pherson forceps are used to harvest the bowman layer, keeping it not dry, not wet (C,D,E,F). Bowman layer is placed in a contact lens for regularizing and cutting with Busin punch (no financial interest) and ready for insertion in the stromal pocket (G,H,I). Video link: https://www.youtube.com/watch?v=TH1-6zRRgfw&t=31s.
After making a 6mm scleral tunnel incision(A,B), mid stromal dissection is performed with red DALK spatula(C), the anterior chamber is filled with air(D), mid stromal dissection with blue DALK spatula(E), and 360 degrees around with white DALK spatula(F), after removal of the larger part of air bubble and the insertion of a Visitec surgical glide into the stromal pocket, a folded bowman layer graft is inserted into this pocket (G,H), and carefully unfolding the bowman layer with a 30 gauge air cannula (I). At the end of the surgical procedure, the bowman layer is sandwiched between the anterior and posterior stromal layers. Video link: https://www.youtube.com/watch?v=_Vb2KqvaVZA
Zaman technique of bowman layer transplantation type I
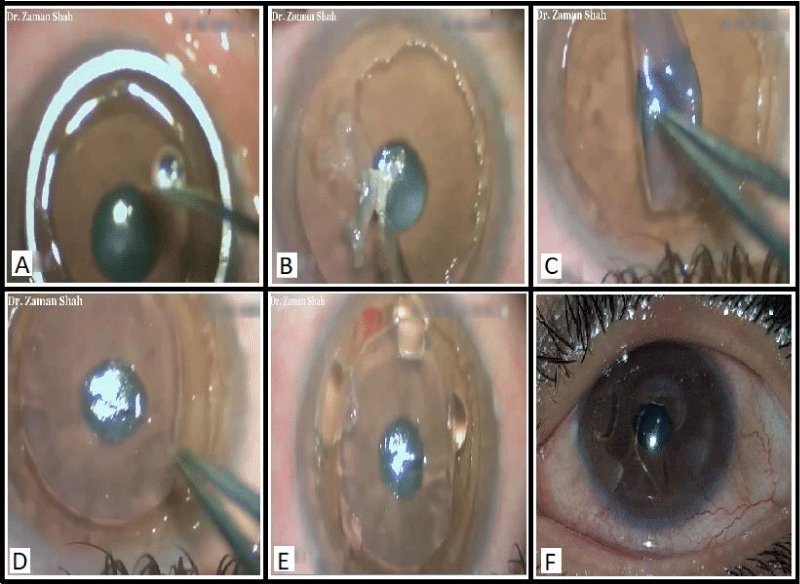
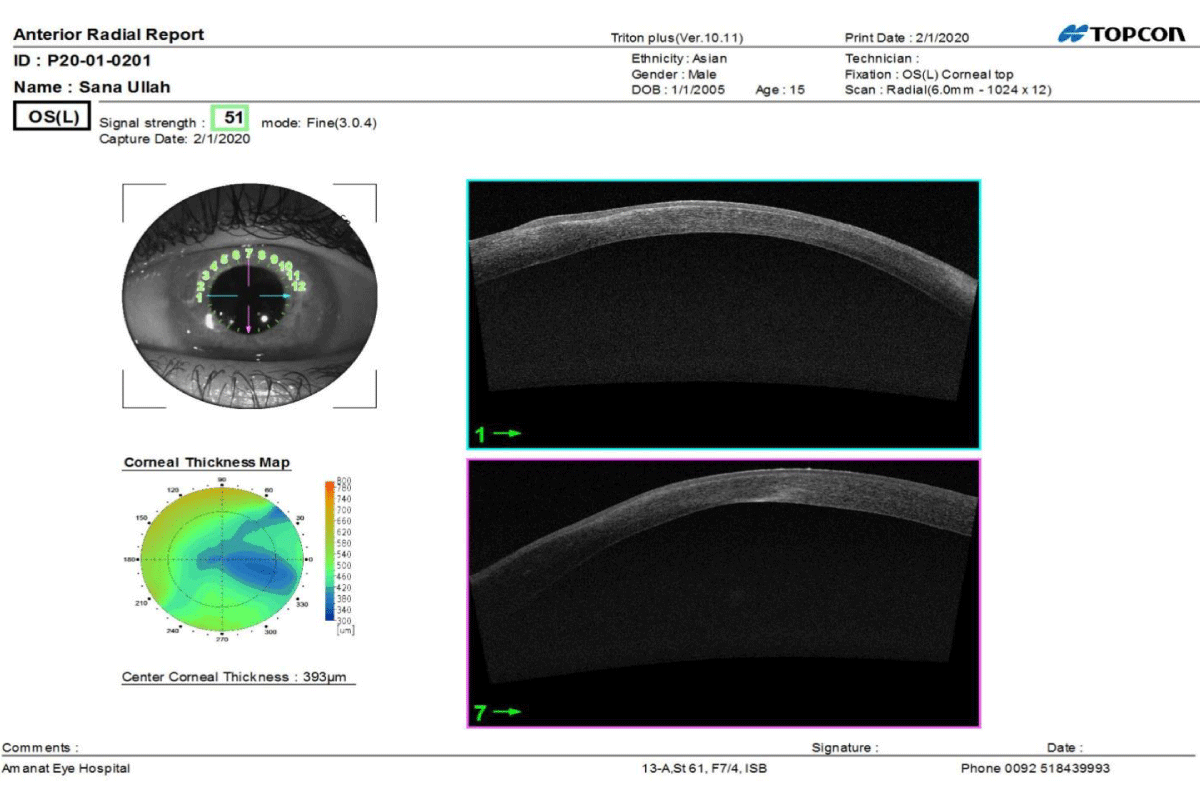
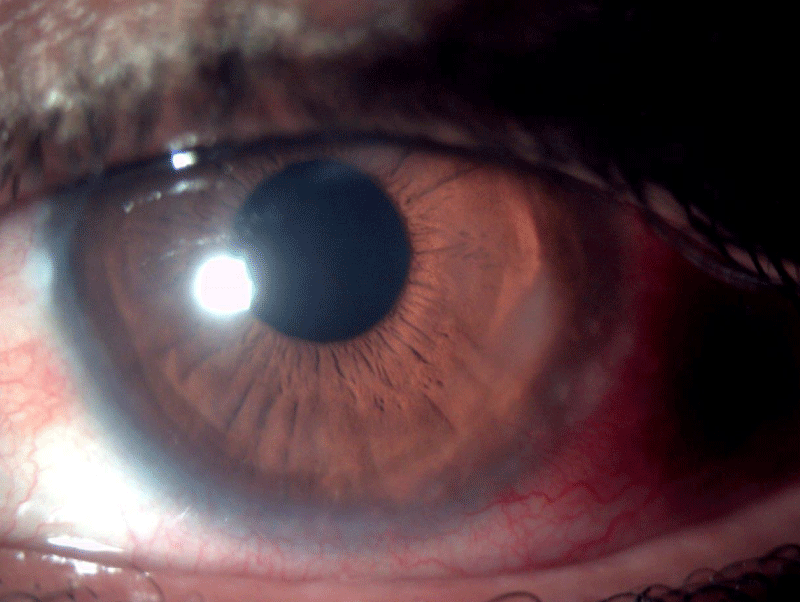
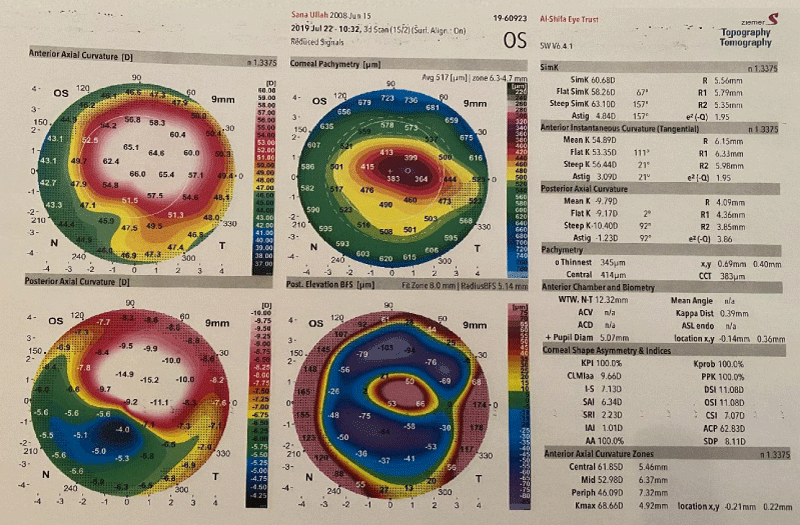
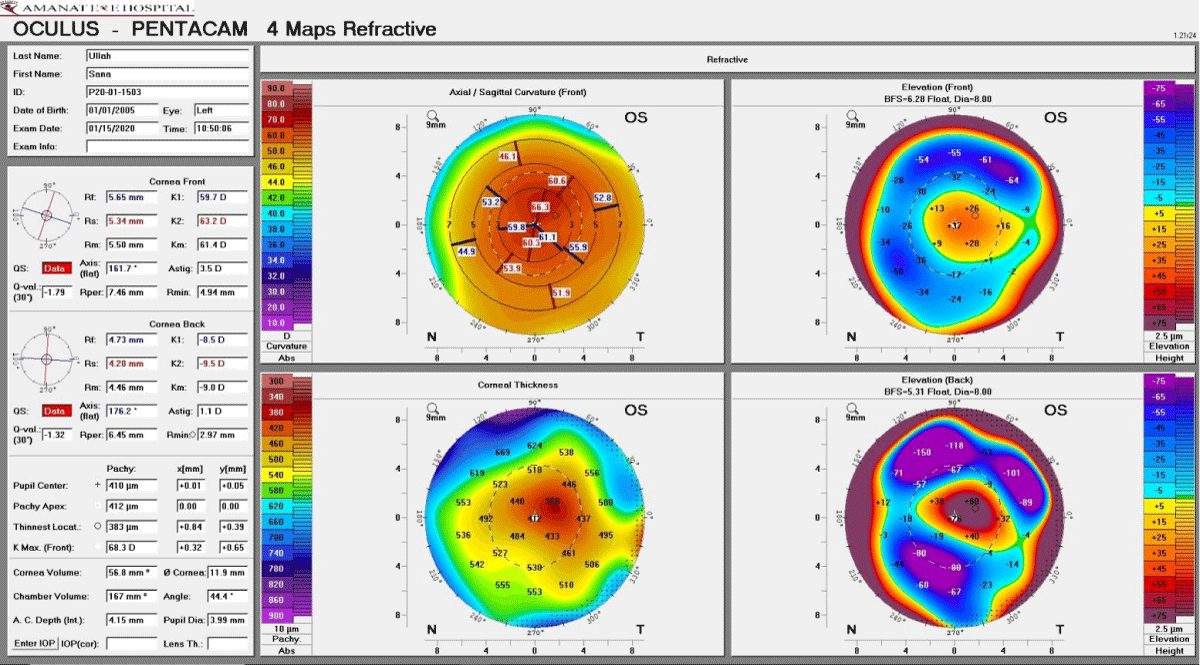
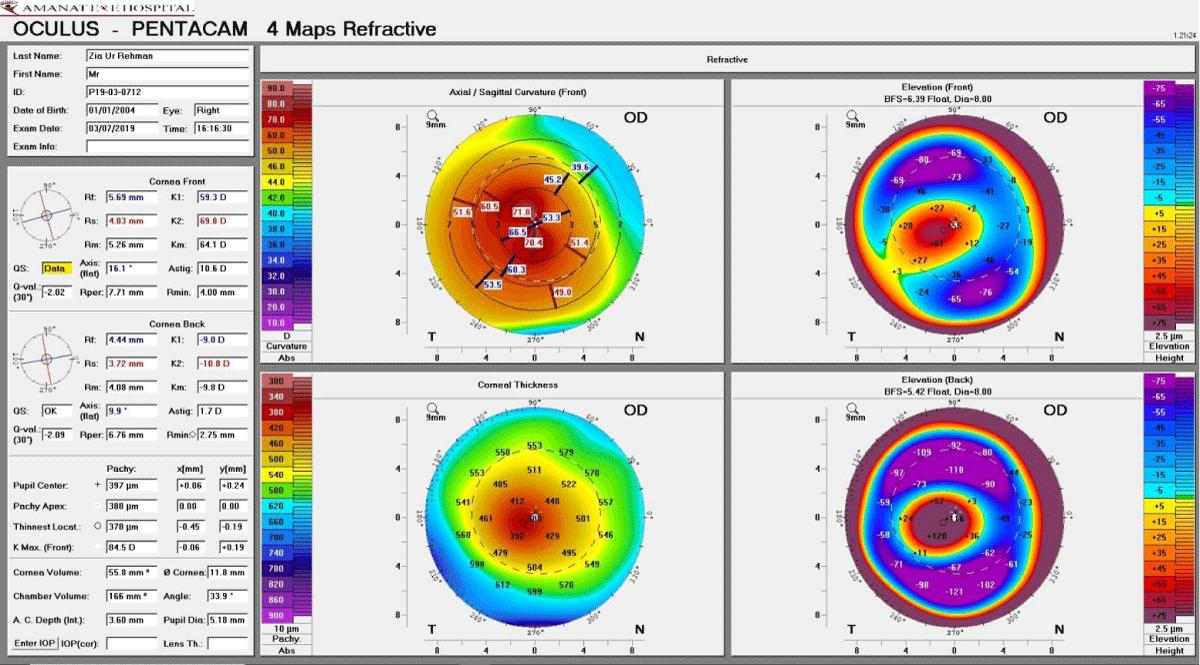
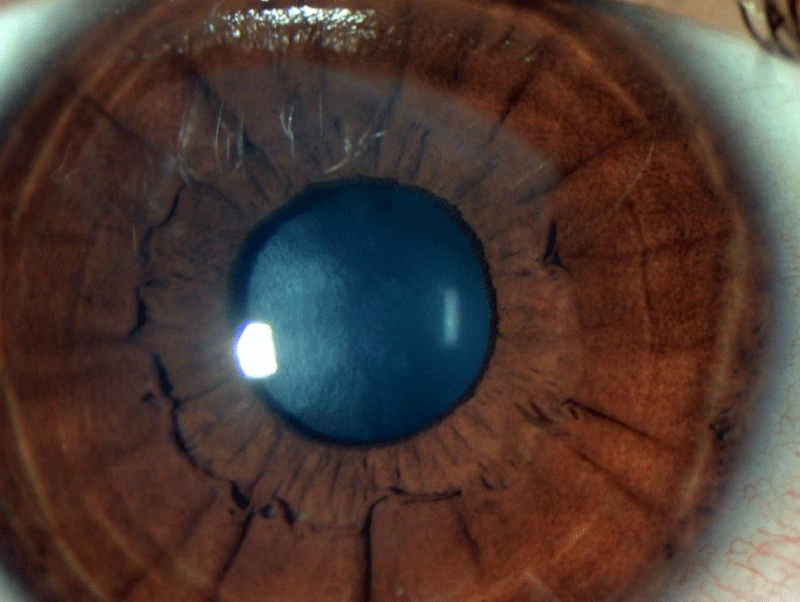
The idea for the Zaman technique was struck upon after it became conceptually evident that electron microscopy shows the breakdown of the BL in advanced keratoconus, which could be construed as an early sign of advanced keratoconus [20]. The type I procedure was performed on topical anesthesia, 70% alcohol, and SPATULA DOUBLE FLAP BURATTO Millennium Number: 87-6871 to de-bride recipient surface epithelium. After harvesting from the donor, the 10 mm BL usually takes a folded configuration. Mostly the epithelial surface of the BL is on the outer surface. The unfolding of BL was carried out on the recipient’s bare stromal beds, keeping in mind the anatomical integrity of BL, i.e., the stromal and epithelial surface of the bowman layer facing their respective stromal and epithelial surfaces of the bare stromal recipient surface. Cyanoacrylate glue was applied on the sides of unfolded BL to avoid dislocation of the un-sutured graft by the eyelid-induced shear forces and to squeeze the BL transplant. Finally, a bandage contact lens was applied (Figure 3). On routine examination up to two and half months follow up, the cyanoacrylate glue was attached with the margins of the BL graft and has created a sort of slopping on the sides and best captured on anterior segment OCT even after 3 months (Figure 5). During this follow-up, foreign body sensation was felt which decreased due to the application of a bandage contact lens. We were uncertain about the growth of the epithelium above or below the BL graft on routine slit-lamp examination (Figure 6), so anterior segment OCT was done after three months which shows clear evidence of the integrity of the BL graft and surface epithelium (Figure 5). It has been noted that even in the presence of cyanoacrylate glue the surface epithelium overrides the transplanted bowman layer. It becomes evident that the unique characteristics of BL do not allow the surface epithelium to grow underneath it. There has been a significant increase in the thinnest location from 345 um pre-op to 383 um post-op day 04 months, 1.3D decrease of topographic astigmatism, while K-max data remained unchanged. Pre-op visual acuity was counting finger (0.04) to 6/24 (0.25) (Figure 7 & 8 and Table 1).
Figure 3: Zaman Technique of bowman layer transplantation type I.
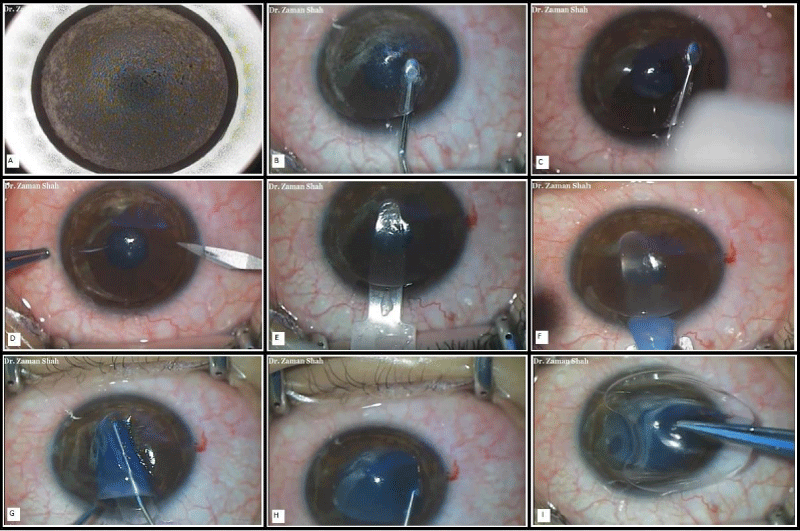
Figure 4: Zaman Technique of bowman layer transplantation type II.
Figure 5: Post-operative Anterior segment OCT of “Zaman Technique of BLT-type I”.
Figure 6: Slit-lamp picture of the “Zaman Technique of BLT-type I”.
Figure 7: Pre op pentacam “Zaman Technique of BLT-type I”.
Figure 8: Post op pentacam “Zaman Technique of BLT-type I”.
| Table 1: Zaman Technique of Bowman Layer Transplantation type 1. | ||||
| Parameter | Pre-op | Post-op day, 4 months | Difference between pre-op to post of day, 4 months | |
| K1 | Cornea Front | 58.26D | 59.7 D | -1.44 D |
| K2 | 63.10D | 63.2 D | 0.1 D | |
| Topo Astigmatism cornea front | 4.84D | 3.5 D | 1.34 D | |
| K1 | Cornea back | -9.17D | -8.5 D | -0.67 D |
| K2 | 10.4D | -9.0 D | -1.4 D | |
| Topo Astigmatism cornea back | -1.23D | 1.1 D | -0.13 D | |
| Thinnest location | 345 um | 383 um | -38 um | |
| K Max | 68.66 D | 68.3 D | 0.33 D | |
| BCVA | CF 1m (0.04) | 6/24(0.25) | ||
Zaman technique of bowman layer transplantation type II
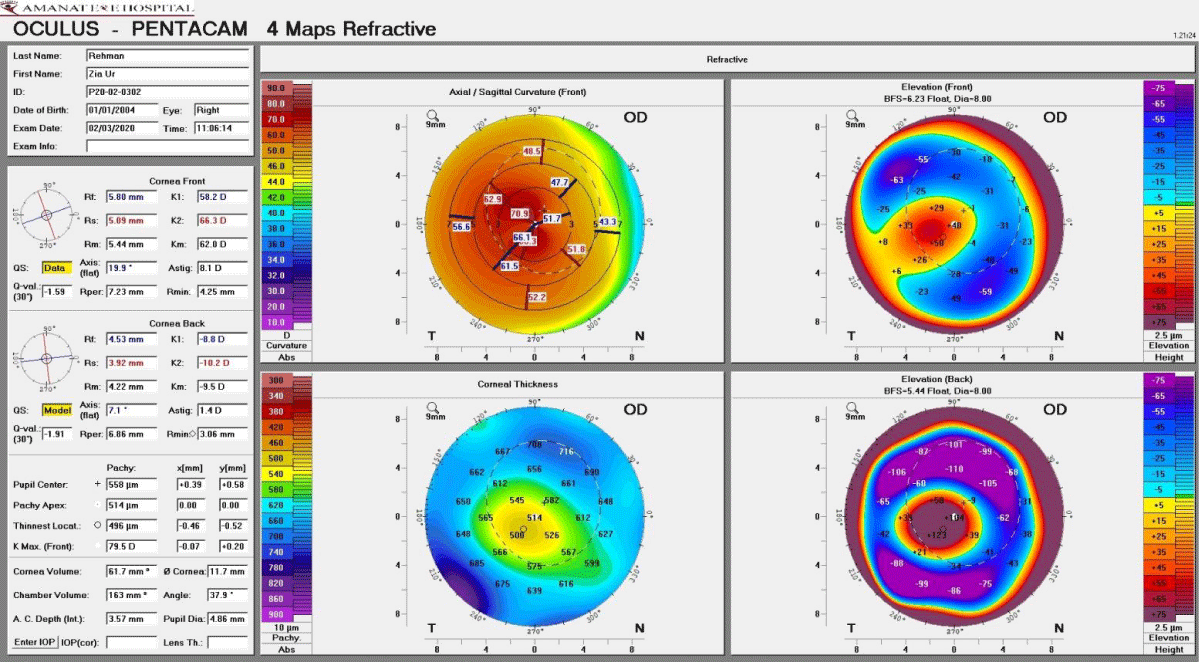
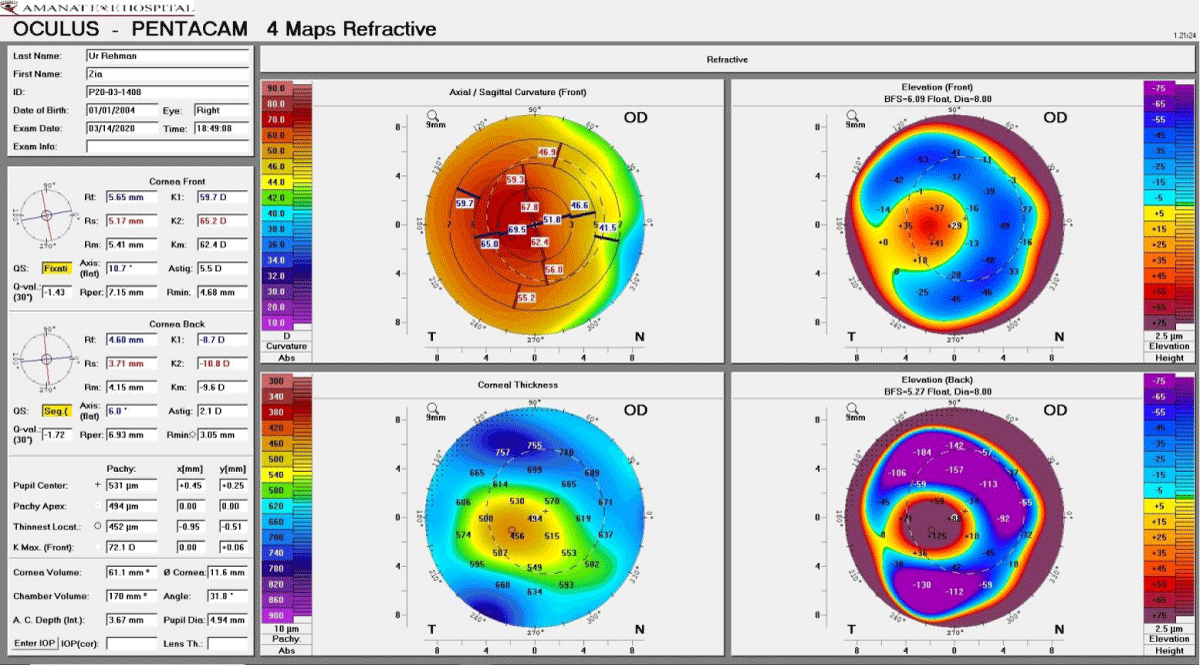
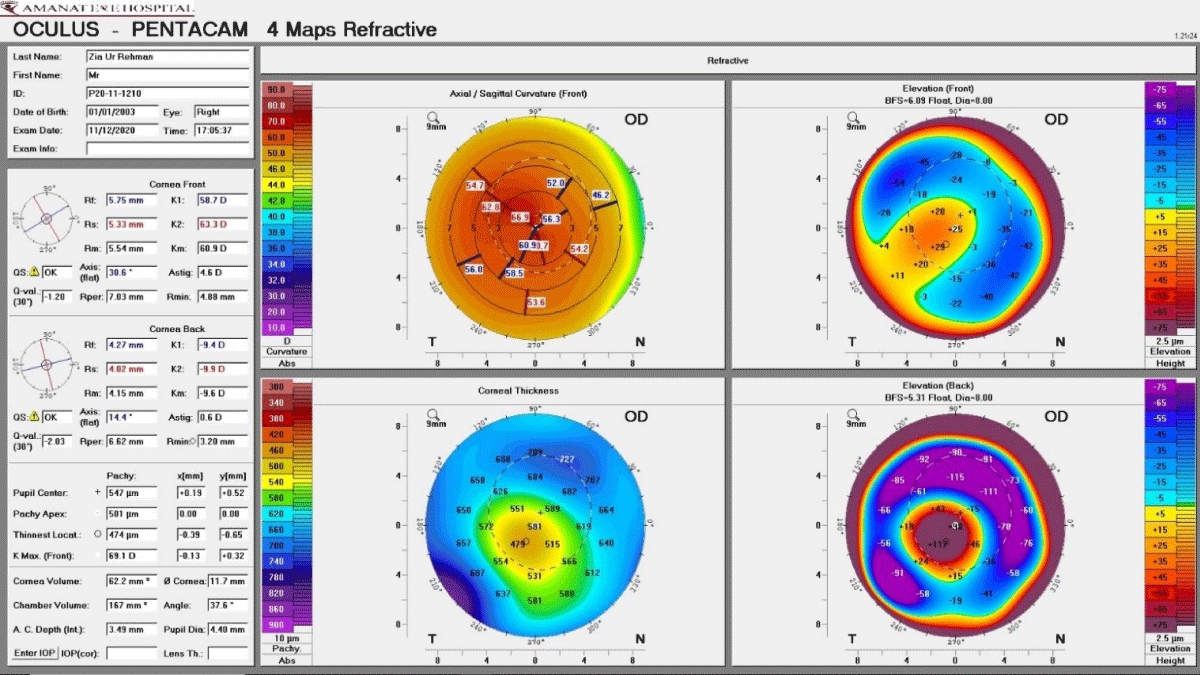
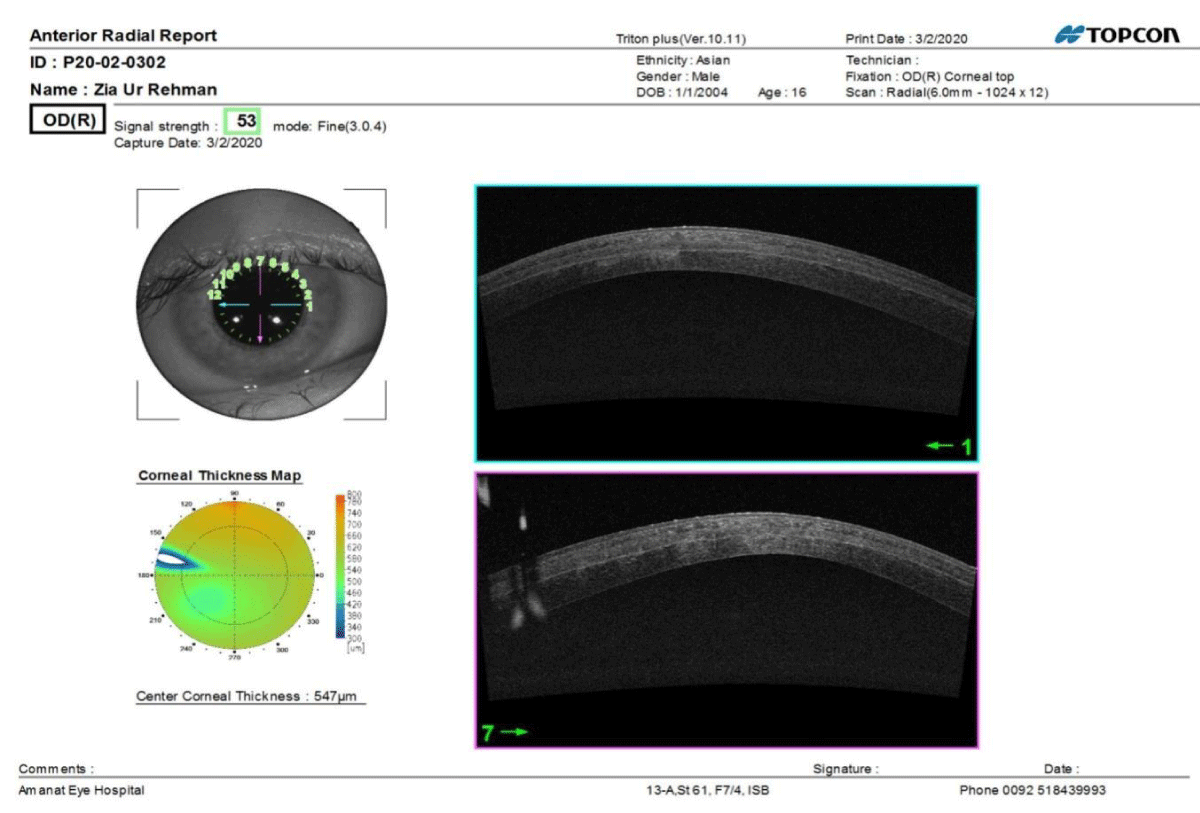
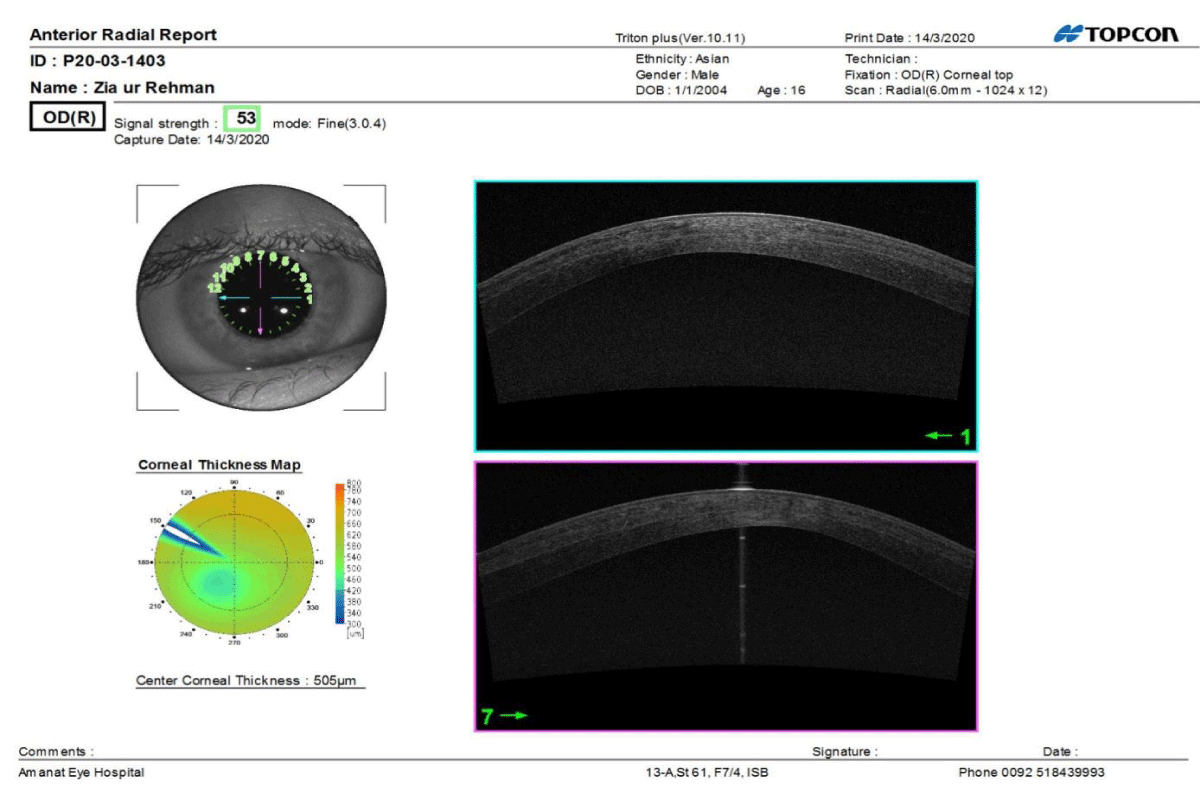
Once the BL graft was prepared, a 10 mm stromal pocket was created at the depth of 150 um very close to the natural anatomical location of BL with a femtosecond laser (VisuMax Carl Zeiss Meditec AG). The entry port was made at 12 o’clock position, two clock hours in size, and created the dissection of the pocket in the same way as in a SMILE technique 3600 around. AC tape was made using a 150 MANI knife which provided space for the BL for easy unfolding. A Visitec surgical glide was inserted into the stromal pocket with the bowman roll on it. The BL was inserted into the stromal pocket and unfolding was done using the cannula with alternate irrigation with BSS and unfolding. Irrigation of the BSS creates room for the unfolding of the bowman layer. Once the BL is completely unfolded, centration is also carried out at the same time with a cannula. The BCL is applied at the end of the procedure (Figure 4). Figure 11a,b shows anterior segment OCT after the second day and one and a half months post-op respectively with comparable thickness, 547 um versus 506um where the BL is sandwiched between the anterior and posterior stromal lamellae in a uniform stromal pocket. Figure 12 shows the slit lamp picture of the first post-op day. Pre-op thinnest location was 378 um, topographic astigmatism 10.6 D and K-max data was 84.5 D (Figure 9). Visual acuity before surgery was CF-1m (0.04). On the first post-operative day, the thinnest location was 496 um, topographic astigmatism was 8.1 and K-max data was 79.5D (Figure 10a). Topographic astigmatism decreased by 2.5D, Kmax decreased by 5D, and the thinnest location increased by 118um (Table 1). After postoperative day 40, the thinnest location was 452 um, astigmatism 5.5 D, and K-max data 71.1 D (Figure 10b). There was a significant reduction of topographic astigmatism by 5.1 D, K-max decreased by 12.4 D, thinnest location increased by 74 um, and BCVA was 6/18 (0.32) (Table 1). The increased thickness of the thinnest location by 74 um was due to the edematous BL and the thickness was even more in the early pantacam due to the hydration and severe insult during harvesting of the BL, i.e., 118 um on the first postoperative day. Although the BL was put in hypertonic saline solution for a few hours before transplantation and preparation of the patient, after 10 months post BLT, the thinnest location increased to 474 um, topo astigmatism to 4.6D, and Kmax to 69.1D (Figure 10c). Topo astigmatism decreased by 6.0D, Kmax decreased by 15.4D, the thinnest location difference was 96 um and BCVA was 6/12 (0.5). Pre-operative cornea back topo astigmatism was 1.70D, which remained the same on the first post-operative day(1.40D), increase to 2.10D on postoperative day 40, and decreased to 0.60 after 10 months. The difference is 1.10D pre-op to post-op 10 months (Table 2).
Figure 9: Pre op pentacam “Zaman Technique of BLT-type II”.
Figure 10a: Post-op pentacam (day 1) “Zaman Technique of BLT-type II”.
Figure 10b: Post-op pentacam (Day 40) “Zaman Technique of BLT-type II”.
Figure 10c: Post-op pentacam (After 10 months) “Zaman Technique of BLT-type II”.
Figure 11a: Post-operative Anterior segment OCT (day 1) “Zaman Technique of BLT-type II”.
Figure 11b: Post-operative Anterior segment OCT (day 40) “Zaman Technique of BLT-type II”.
Figure 12: Slit-lamp picture of the “Zaman Technique of BLT-type II”. (Post-op day 1).
| Table 2: Zaman Technique of Bowman Layer Transplantation type 2. | ||||||||
| Parameter | Pre-op | Post-op, day 1 | Difference Btw Pre-op and post-op, day 1 | Post-op, day 40 | Difference Btw Pre-op and post-op, day 40 | Post-op after 10 months | Difference Btw Pre-op and post-op, 10 months | |
| K1 | Cornea Front | 59.3 D | 58.2 D | 1.1 D | 46.4 D | 12.9 D | 58.7 | 0.6 |
| K2 | 69.8 D | 66.3 D | 3.5 D | 52.1 D | 17.7 D | 63.3 | 6.5 | |
| Topo astigmatism cornea front | 10.60D | 8.1 D | 2.5 D | 5.5 D | 5.1 D | 4.60D | 6.0D | |
| K1 | Cornea Back | -9.00 D | -8.8 D | -1.2 D | -8.70 D | -1.3 D | -9.4 D | 0.4 D |
| K2 | -10.80 D | -10.2 D | -0.60 D | -10.80 D | 0.0 D | -9.9 D | 0.9 D | |
| Topo astigmatism cornea back | 1.7 D | 1.4 D | 0.3 D | 2.1 D | +0.4 D | 0.6 D | 1.1 D | |
| Thinnest location | 378 um | 496 um | +115 | 452 um | +76 | 474 um | +96 um | |
| K-max | 84.5 D | 79.5 D | 5 D | 72.1 D | 12.4 D | 69.10 D | 15.4 D | |
| BCVA | CF 1 meter(0.04) | 6/36 (0.16) | 6/18 (0.32) | 6/12 (0.5) | ||||
LASEK TREPHINE & ALCOHOL RET. WELL 10 mm (A), debridement of surface epithelium with SPATULA DOUBLE FLAP BURATTO Millennium Number: 87-6871 (B), folded BL placed on bare recipient stromal bed (C), spreading of BL on the stromal bed (D), application of cyanoacrylate glue (E), Post-operative picture after 3 months (F). Video link: https://www.youtube.com/watch?v=TH1-6zRRgfw
Creation of stromal pocket with VisuMax Carl Zeiss Meditec AG Femtosecond laser, (A), dissection of mid stromal pocket with a SMILE spatula (B), 3600 around mid stromal dissection with SMILE spatula (C), AC tap with 150 MANI knife (D), placement of visitec surgical glide in the mid stromal pocket (E), BL role is placed on surgical glide (F), insertion of the graft into the stromal pocket (G), unrolling of BL with canula (H), application of BCL (I). Video link: https://www.youtube.com/watch?v=L5imRoCv_84
BL is an acellular and non-regenerating layer that is composed of dense randomly arranged collagen fibrils. The anterior surface is toward the epithelium and the stromal surface merges with the collagen of the anterior corneal stroma. BL is 10-15 um in thickness which decreases with advancing age [21,22]. Electron microscopy has shown that in advanced keratoconus, there is disruption, ruptures, gaps, and scaring of BL [23,24]. Keeping this idea in mind, the Zaman Technique of BLT type I was designed to replace the disrupted BL with a healthy donor BL in the natural anatomical location using fibrin glue at the graft margin for adhesion which gives anatomical strength to the recipient cornea and also flattens it. Van Dijk, et al. theorized that implanting a donor BL in the mid-stroma could restore the shape and strength of the cornea effectively by pulling the anterior corneal surface flatter [26]. The function of the BL is still unclear but studies have determined its possible role against ultraviolet, being a barrier against microbial infection, and having strong biomechanical properties [25,26]. Bowman layer is disrupted by photorefractive keratectomy which decreases the corneal biomechanical properties.
The results of the Zaman technique on 19 eyes after BLT, and 18 months of follow-up, have shown that the corrected distance visual acuity remarkably improved and remained stable in 90% of cases. The level of contact lens tolerance was measured at 100% post-operatively, which allowed full-day wear. There has also been an increase in the thinnest point pachymetry. K-max decreased by more than 12 D and mean K reduced by 8 D. Furthermore, the mean endothelial cell density did not change after surgery. The risk of graft rejection is extremely minimal due to an acellular material transplanted [28].
Some of the recorded complications of BLT have been the tearing of the BL during harvesting, which was there up to 30%, and the failure to acquire a required thickness of the BL graft, which has been recorded at 3% [29]. During the procedure, the worst procedure is the Descemet membrane micro-perforation (10%) [30].
To lower the risk of intraoperative perforation, the Zaman Technique of BLT type II was designed for dissecting the stromal pocket using Femtosecond Laser with minimal damage at a depth of 150 um to properly place and unfold the BL graft. In the old method of bowman layer transplantation, there had been a 10% chance of Descemet perforation and in the case of macro-perforation, the procedure could be converted to penetrating keratoplasty. In the Zaman Technique, the chance of perforation is negligible, almost 0%. Contact lens tolerance, mean K value, K max data, and thinnest point pachymetry results have been the same as that of the old technique of BLT. For the last many years, Femtosecond Laser has been used in various refractive procedures such as Lasik, SMILE, intracorneal ring segment, corneal inlay for presbyopic correction, corneal lamellar transplant procedure, and cataract surgery [31-33].
The use of a Femtosecond Laser is much safer for the creation of a stromal pocket while avoiding the use of a traditional microkeratome blade [34]. Flap thickness, regularity, and diameter in femtosecond laser have been shown to have good results than in microkeratome assisted flap [35]. Similarly, the complications rate like dry eyes, risk for flap hole and free flap are reduced [36].
In the Zaman Technique of bowman layer transplantation type II, there has been an increase in thickness of the thinnest location postoperatively. On the second post-op day, it increased by 118 um which reduced to 74 um after one and half months. It was noted during implantation that the thicker graft was easy to implant and unfold. It is very difficult to obtain the sole bowman layer as anterior stromal tissue closely adheres to it. Other authors have also described such an increase in corneal thickness suggesting that donor tissue encompasses anterior stroma. As suggested by Galvis, et al. [37], the remaining stroma might reduce the risk of tearing the bowman layer because it is easier to obtain a lamellar portion of the anterior corneal stroma.
The femtosecond laser has also been used in various corneal transplantation procedures like DALK, and intracorneal ring segment (ICRS) [38,39]. That is why femtosecond laser was used to design this new technique of corneal transplantation due to its regular cut on uneven and irregular corneal thickness.
So far we have performed only one case using the Zaman Technique Type II with a femtosecond laser at a depth of 150 um. The BL is programmed to be placed at various depths in more cases. Keeping in mind the safety and accuracy of the femtosecond laser, we would be able to create a stromal pocket at different depths concerning safety, biocompatibility, and efficiency during Bowman layer transplantation. We would be able to get BL from the whole globe prepared by femtosecond laser, which could be a thicker and regular lamellar portion of the anterior cornea than prepared manually [40].
Both Zaman techniques of bowman layer transplantation are the unique surgical treatment of advanced keratoconus with progressive ectasia and have progressively shown that they can stabilize the keratoconus and improve visual acuity, which allows for a better contact lens tolerance while the risk of complications is negligible and postpones the need for penetrating or deep anterior lamellar keratoplasty. The femtosecond laser provides an option for BLT to obtain better results regarding accuracy, safety, and reproducibility. Similarly, fibrin glue can also be used for BLT to obtain structural and anatomical stability.
Complaints about ethical standards
Both patients signed an IRB-approved informed consent. The study conforms to the criteria laid down by the Declaration of Helsinki.
Conflict of interest: The authors Dr. Zaman Shah and other co-authors have no financial interest or have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in the manuscript.
- Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998 Jan-Feb;42(4):297-319. doi: 10.1016/s0039-6257(97)00119-7. PMID: 9493273.
- Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003 May;135(5):620-7. doi: 10.1016/s0002-9394(02)02220-1. PMID: 12719068.
- Raiskup F, Spoerl E. Corneal cross-linking with hypo-osmolar riboflavin solution in thin keratoconic corneas. Am J Ophthalmol. 2011 Jul;152(1):28-32.e1. doi: 10.1016/j.ajo.2011.01.016. Epub 2011 May 6. PMID: 21529763.
- Sloot F, Soeters N, van der Valk R, Tahzib NG. Effective corneal collagen crosslinking in advanced cases of progressive keratoconus. J Cataract Refract Surg. 2013 Aug;39(8):1141-5. doi: 10.1016/j.jcrs.2013.01.045. Epub 2013 May 24. PMID: 23711873.
- Alio JL, Vega-Estrada A, Esperanza S, Barraquer RI, Teus MA, Murta J. Intrastromal corneal ring segments: how successful is the surgical treatment of keratoconus? Middle East Afr J Ophthalmol. 2014 Jan-Mar;21(1):3-9. doi: 10.4103/0974-9233.124076. PMID: 24669139; PMCID: PMC3959038.
- Christo CG, van Rooij J, Geerards AJ, Remeijer L, Beekhuis WH. Suture-related complications following keratoplasty: a 5-year retrospective study. Cornea. 2001 Nov;20(8):816-9. doi: 10.1097/00003226-200111000-00008. PMID: 11685058.
- Kelly TL, Williams KA, Coster DJ; Australian Corneal Graft Registry. Corneal transplantation for keratoconus: a registry study. Arch Ophthalmol. 2011 Jun;129(6):691-7. doi: 10.1001/archophthalmol.2011.7. Epub 2011 Feb 14. PMID: 21320951.
- Tan DT, Dart JK, Holland EJ, Kinoshita S. Corneal transplantation. Lancet. 2012 May 5;379(9827):1749-61. doi: 10.1016/S0140-6736(12)60437-1. PMID: 22559901.
- Lake D, Hamada S, Khan S, Daya SM. Deep anterior lamellar keratoplasty over penetrating keratoplasty for host rim thinning and ectasia. Cornea. 2009 Jun;28(5):489-92. doi: 10.1097/ICO.0b013e31818d3b3c. PMID: 19421052.
- Speaker MG, Arentsen JJ, Laibson PR. Long-term survival of large diameter penetrating keratoplasties for keratoconus and pellucid marginal degeneration. Acta Ophthalmol Suppl. 1989;192:17-9. doi: 10.1111/j.1755-3768.1989.tb07089.x. PMID: 2554648.
- Abou Shousha M, Perez VL, Fraga Santini Canto AP, Vaddavalli PK, Sayyad FE, Cabot F, Feuer WJ, Wang J, Yoo SH. The use of Bowman's layer vertical topographic thickness map in the diagnosis of keratoconus. Ophthalmology. 2014 May;121(5):988-93. doi: 10.1016/j.ophtha.2013.11.034. Epub 2014 Jan 24. PMID: 24468653; PMCID: PMC4011960.
- van Dijk K, Parker J, Tong CM, Ham L, Lie JT, Groeneveld-van Beek EA, Melles GR. Midstromal isolated Bowman layer graft for reduction of advanced keratoconus: a technique to postpone penetrating or deep anterior lamellar keratoplasty. JAMA Ophthalmol. 2014 Apr 1;132(4):495-501. doi: 10.1001/jamaophthalmol.2013.5841. PMID: 24557359.
- Melles GR, Binder PS. A comparison of wound healing in sutured and unsutured corneal wounds. Arch Ophthalmol. 1990 Oct;108(10):1460-9. doi: 10.1001/archopht.1990.01070120108039. PMID: 2222279.
- Melles GR, Binder PS, Anderson JA. Variation in healing throughout the depth of long-term, unsutured, corneal wounds in human autopsy specimens and monkeys. Arch Ophthalmol. 1994 Jan;112(1):100-9. doi: 10.1001/archopht.1994.01090130110027. PMID: 8285876.
- Alió JL, Shabayek MH. Corneal higher order aberrations: a method to grade keratoconus. J Refract Surg. 2006 Jun;22(6):539-45. doi: 10.3928/1081-597X-20060601-05. PMID: 16805116.
- Koh S, Maeda N, Nakagawa T, Nishida K. Quality of vision in eyes after selective lamellar keratoplasty. Cornea. 2012 Nov;31 Suppl 1:S45-9. doi: 10.1097/ICO.0b013e318269c9cd. PMID: 23038035.
- Oculus Optikgeräte GmbH. Oculus Pentacam instruction manual: measurement and evaluation system for the anterior segment of the eye. Wetzlar, Germany: Oculus Optikgeräte GmbH; 2005.
- van Dijk K, Parker J, Tong CM, Ham L, Lie JT, Groeneveld-van Beek EA, Melles GR. Midstromal isolated Bowman layer graft for reduction of advanced keratoconus: a technique to postpone penetrating or deep anterior lamellar keratoplasty. JAMA Ophthalmol. 2014 Apr 1;132(4):495-501. doi: 10.1001/jamaophthalmol.2013.5841. PMID: 24557359.
- Lie J, Droutsas K, Ham L, Dapena I, Ververs B, Otten H, van der Wees J, Melles GR. Isolated Bowman layer transplantation to manage persistent subepithelial haze after excimer laser surface ablation. J Cataract Refract Surg. 2010 Jun;36(6):1036-41. doi: 10.1016/j.jcrs.2010.03.032. PMID: 20494779.
- Sawaguchi S, Fukuchi T, Abe H, Kaiya T, Sugar J, Yue BY. Three-dimensional scanning electron microscopic study of keratoconus corneas. Arch Ophthalmol. 1998 Jan;116(1):62-8. doi: 10.1001/archopht.116.1.62. PMID: 9445209.
- Gipson IK, Joyce NC, Zieske JD. The anatomy and cell biology of the human cornea, limbus, conjunctiva and adnexa. In: Foster CS, Azar D, Dolhman CH, eds, The Cornea. Philadelphia, PA, Lippincott, Williams & Wilkins, 2004; 1–35.
- Germundsson J, Karanis G, Fagerholm P, Lagali N. Age-related thinning of Bowman's layer in the human cornea in vivo. Invest Ophthalmol Vis Sci. 2013 Sep 11;54(9):6143-9. doi: 10.1167/iovs.13-12535. PMID: 23970471.
- Tuori AJ, Virtanen I, Aine E, Kalluri R, Miner JH, Uusitalo HM. The immunohistochemical composition of corneal basement membrane in keratoconus. Curr Eye Res. 1997 Aug;16(8):792-801. doi: 10.1076/ceyr.16.8.792.8989. PMID: 9255508.
- Sawaguchi S, Fukuchi T, Abe H, Kaiya T, Sugar J, Yue BY. Three-dimensional scanning electron microscopic study of keratoconus corneas. Arch Ophthalmol. 1998 Jan;116(1):62-8. doi: 10.1001/archopht.116.1.62. PMID: 9445209.
- Boote C, Du Y, Morgan S, Harris J, Kamma-Lorger CS, Hayes S, Lathrop KL, Roh DS, Burrow MK, Hiller J, Terrill NJ, Funderburgh JL, Meek KM. Quantitative assessment of ultrastructure and light scatter in mouse corneal debridement wounds. Invest Ophthalmol Vis Sci. 2012 May 14;53(6):2786-95. doi: 10.1167/iovs.11-9305. PMID: 22467580; PMCID: PMC3367468.
- Grieve K, Georgeon C, Andreiuolo F, Borderie M, Ghoubay D, Rault J, Borderie VM. Imaging Microscopic Features of Keratoconic Corneal Morphology. Cornea. 2016 Dec;35(12):1621-1630. doi: 10.1097/ICO.0000000000000979. PMID: 27560027; PMCID: PMC5094201.
- van Dijk K, Parker J, Tong CM, Ham L, Lie JT, Groeneveld-van Beek EA, Melles GR. Midstromal isolated Bowman layer graft for reduction of advanced keratoconus: a technique to postpone penetrating or deep anterior lamellar keratoplasty. JAMA Ophthalmol. 2014 Apr 1;132(4):495-501. doi: 10.1001/jamaophthalmol.2013.5841. PMID: 24557359.
- van Dijk K, Parker JS, Baydoun L, Ilyas A, Dapena I, Groeneveld-van Beek EA, Melles GRJ. Bowman layer transplantation: 5-year results. Graefes Arch Clin Exp Ophthalmol. 2018 Jun;256(6):1151-1158. doi: 10.1007/s00417-018-3927-7. Epub 2018 Feb 14. PMID: 29445872.
- Groeneveld-van Beek EA, Parker J, Lie JT, Bourgonje V, Ham L, van Dijk K, van der Wees J, Melles GR. Donor Tissue Preparation for Bowman Layer Transplantation. Cornea. 2016 Dec;35(12):1499-1502. doi: 10.1097/ICO.0000000000000905. PMID: 27362885.
- van Dijk K, Liarakos VS, Parker J, Ham L, Lie JT, Groeneveld-van Beek EA, Melles GR. Bowman layer transplantation to reduce and stabilize progressive, advanced keratoconus. Ophthalmology. 2015 May;122(5):909-17. doi: 10.1016/j.ophtha.2014.12.005. Epub 2015 Jan 14. PMID: 25596620.
- Aristeidou A, Taniguchi EV, Tsatsos M, Muller R, McAlinden C, Pineda R, Paschalis EI. The evolution of corneal and refractive surgery with the femtosecond laser. Eye Vis (Lond). 2015 Jul 14;2:12. doi: 10.1186/s40662-015-0022-6. PMID: 26605365; PMCID: PMC4655461.
- Ibrahim T, Goernert P, Rocha G. Femto-second laser (FSL) techniques and consistency in corneal surgery: experimental study. Can J Ophthalmol. 2018 Aug;53(4):324-329. doi: 10.1016/j.jcjo.2017.11.005. Epub 2018 Apr 2. PMID: 30119784.
- Grewal DS, Schultz T, Basti S, Dick HB. Femtosecond laser-assisted cataract surgery--current status and future directions. Surv Ophthalmol. 2016 Mar-Apr;61(2):103-31. doi: 10.1016/j.survophthal.2015.09.002. Epub 2015 Sep 26. PMID: 26409902.
- Aristeidou A, Taniguchi EV, Tsatsos M, Muller R, McAlinden C, Pineda R, Paschalis EI. The evolution of corneal and refractive surgery with the femtosecond laser. Eye Vis (Lond). 2015 Jul 14;2:12. doi: 10.1186/s40662-015-0022-6. PMID: 26605365; PMCID: PMC4655461.
- Pajic B, Vastardis I, Pajic-Eggspuehler B, Gatzioufas Z, Hafezi F. Femtosecond laser versus mechanical microkeratome-assisted flap creation for LASIK: a prospective, randomized, paired-eye study. Clin Ophthalmol. 2014 Sep 22;8:1883-9. doi: 10.2147/OPTH.S68124. PMID: 25284975; PMCID: PMC4181739.
- Moshirfar M, Gardiner JP, Schliesser JA, Espandar L, Feiz V, Mifflin MD, Chang JC. Laser in situ keratomileusis flap complications using mechanical microkeratome versus femtosecond laser: retrospective comparison. J Cataract Refract Surg. 2010 Nov;36(11):1925-33. doi: 10.1016/j.jcrs.2010.05.027. PMID: 21029902.
- Galvis V, Tello A, Carreño NI, Berrospi RD, Niño CA, Leiva F. Keratoconus and Bowman Layer Transplantation. Cornea. 2017 Mar;36(3):e8. doi: 10.1097/ICO.0000000000001142. PMID: 28079692.
- Lu Y, Shi YH, Yang LP, Ge YR, Chen XF, Wu Y, Huang ZP. Femtosecond laser-assisted deep anterior lamellar keratoplasty for keratoconus and keratectasia. Int J Ophthalmol. 2014 Aug 18;7(4):638-43. doi: 10.3980/j.issn.2222-3959.2014.04.09. PMID: 25161934; PMCID: PMC4137198.
- Jabbarvand M, Salamatrad A, Hashemian H, Mazloumi M, Khodaparast M. Continuous intracorneal ring implantation for keratoconus using a femtosecond laser. J Cataract Refract Surg. 2013 Jul;39(7):1081-7. doi: 10.1016/j.jcrs.2013.02.054. Epub 2013 May 22. PMID: 23706931.
- Groeneveld-van Beek EA, Parker J, Lie JT, Bourgonje V, Ham L, van Dijk K, van der Wees J, Melles GR. Donor Tissue Preparation for Bowman Layer Transplantation. Cornea. 2016 Dec;35(12):1499-1502. doi: 10.1097/ICO.0000000000000905. PMID: 27362885.