More Information
Submitted: December 07, 2023 | Approved: December 26, 2023 | Published: December 27, 2023
How to cite this article: Bouayad A, Khodriss C, Tantani S, Fadel H, Rachidi SA, et al. Celiac disease in a teenager revealed with Wernicke Encephalopathy. Int J Clin Exp Ophthalmol. 2023; 7: 011-014.
DOI: 10.29328/journal.ijceo.1001054
Copyright Licence: © 2023 Bouayad A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Nystagmus; Bilateral sixth nerve palsy; Celiac disease; Thiamine wernicke’s encephalopathy
Celiac disease in a teenager revealed with Wernicke Encephalopathy
Amira Bouayad1,2*, Chaimae Khodriss1,2, Sihame Tantani3, Hicham Fadel4, Siham Alaoui Rachidi1,5 and Meriem Elbahloul1,2
1Faculty of Medicine and Pharmacy Tangier, Abdelmalek Essaâdi University, Tangier, Morocco
2Department of Ophthalmology, Mohammed 6 University Hospital of Tangier, Morocco
3Department of Pediatrics, Mohammed 5 Hospital of Tangier, Morocco
4Department of Neurology, Al Kortobi Hospital of Tangier, Morocco
5Department of Radiology, University Hospital of Tangier, Morocco
*Address for Correspondence: Amira Bouayad, Faculty of Medicine and Pharmacy Tangier, Abdelmalek Essaâdi Department of Ophthalmology, Mohammed 6 University Hospital of Tangier, Morocco, Email: [email protected]
Background: Wernicke encephalopathy is an acute neurological condition defined by a clinical triad of ophthalmoplegia, ataxia, and confusion. This disease is due to thiamine deficiency.
Case presentation: After persistent diarrhea and vomiting, a 15-year-old boy presented up-beating nystagmus, with binocular vertical diplopia and unstable gait. An etiological workup revealed a celiac disease. Magnetic resonance imaging showed bilateral periaqueductal region lesions.
Treatment and discussion: Because of suspected Wernicke’s encephalopathy, the patient was treated with thiamine replacement and significant improvement of symptoms took place. Wernicke encephalopathy is a serious medical disorder with enormous morbidity and mortality. Evaluation should include patient history with a physical and ophthalmologic examination and laboratory workup with appropriate imaging.
Conclusion: Undiagnosed celiac disease can lead to malabsorption of vitamin B1 causing acute symptoms of Wernicke encephalopathy.
Wernicke encephalopathy (WE) is a neurological emergency resulting from thiamine deficiency. It presents with varied neurocognitive manifestations, typically involving mental status changes, gait, and oculomotor dysfunction [1]. The prevalence of WE in the general population is approximated from 0.4% to 2.8% [2]. And it carries an approximated 20% mortality [1].
It is a disease that is usually, but not entirely seen in those with persistent alcohol excess [1]. Among the other causes, celiac disease is an immune-mediated situation characterized by small intestinal enteropathy and systemic symptoms due to malabsorption and/or immune activation [3].
Successful management of this disease requires early identification and efficient medical interventions to prevent the high morbidity and mortality associated with this disease. Hence, we hereby report a case of celiac disease recognized by Wernicke encephalopathy.
We report the case of a teenager with Wernicke encephalopathy complicating celiac disease.
A 15-year-old boy presented to the emergency department with a 3-day history of binocular vertical diplopia and unstable gait. His previous ocular history was unremarkable. His medical history was significant for treating Helicobacter pylori gastritis ‘with infection eradication therapy’ and uncontrollable vomiting and diarrhea. There is no history of toxic habits that were mentioned. His family medical and ocular histories were noncontributory.
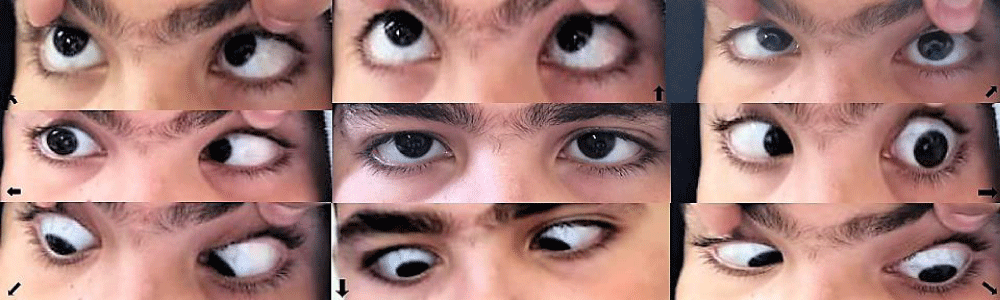
Upon ocular examination, his visual acuity(VA) measured 20/20 in both eyes, ocular motility examination revealed small amplitude and moderate frequency up-beating nystagmus that increased slightly on lateral gaze, on up gaze, and on downgaze and a bilateral sixth cranial nerve palsy (Figure 1). Pupillary light reflexes were brisk with no relative afferent pupil defect. Biomicroscopy found normal anterior segment structures. Dilated fundus evaluation was normal, including both optic nerve appearances.
Figure 1: Ocular motility examination revealing bilateral sixth cranial nerve palsy.
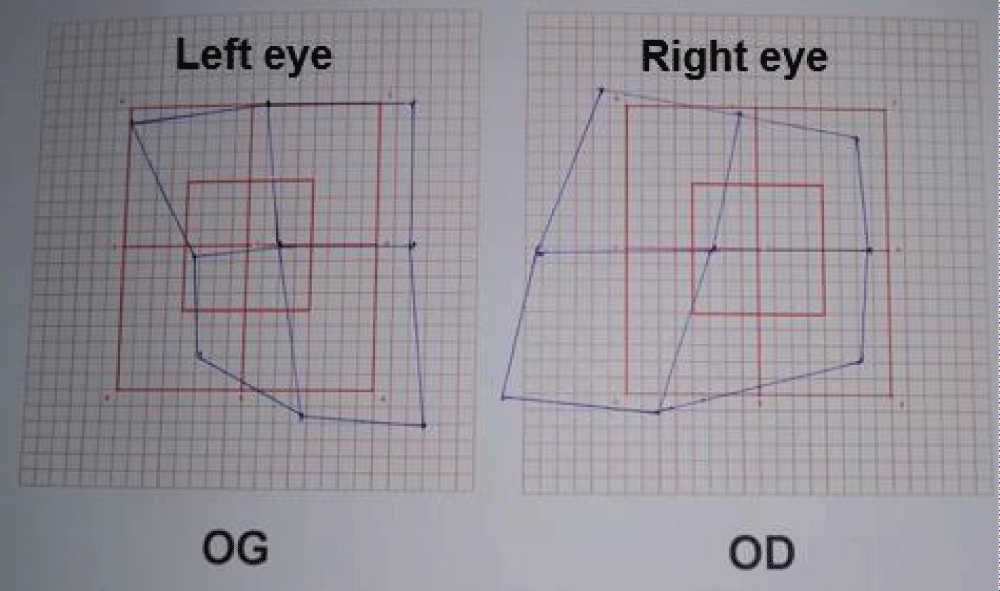
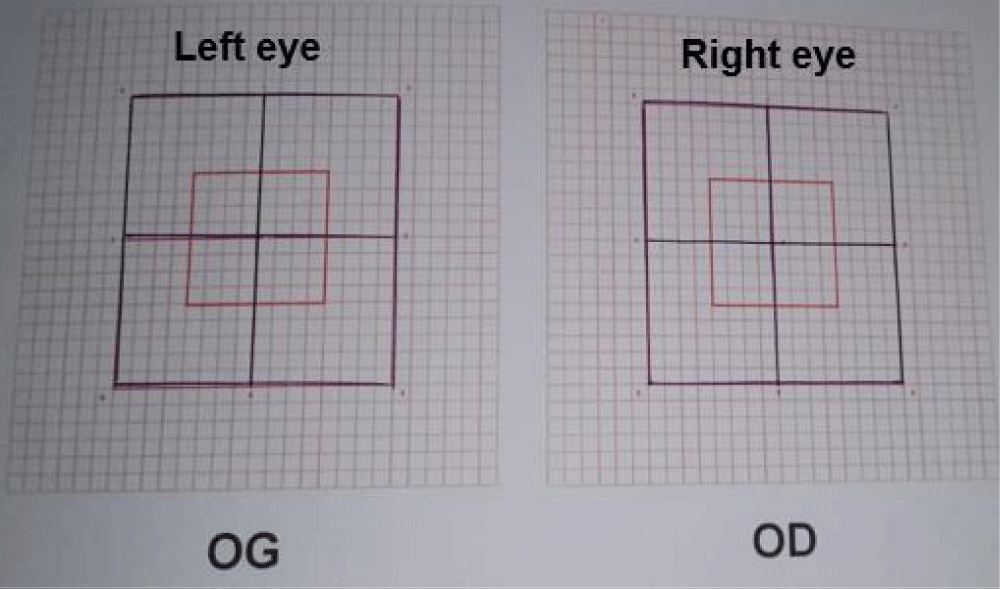
A Lancaster Test confirmed the bilateral sixth cranial nerve palsy, classified as stage 3 (Figure 2).
Figure 2: Lancaster test showing the bilateral sixth cranial nerve palsy.
On general examination, the patient was apyrexic, asthenic, and anorexic, and had a normal heart rate, and hypotension of 100/60mmHg. He had puberty delay and epigastric tenderness.
Neurological examination revealed an ataxic gait, tendon reflexes, and muscle strength were normal. There were no signs of confusion or delirium. There were no focal neurological signs, but a slight decrease in proprioceptive sensation especially vibratory sensitivity in lower limbs. The remaining cranial nerves were intact.
An etiologic work-up, which included an upper-gastrointestinal endoscopy with biopsy that revealed chronic gastritis and celiac disease.
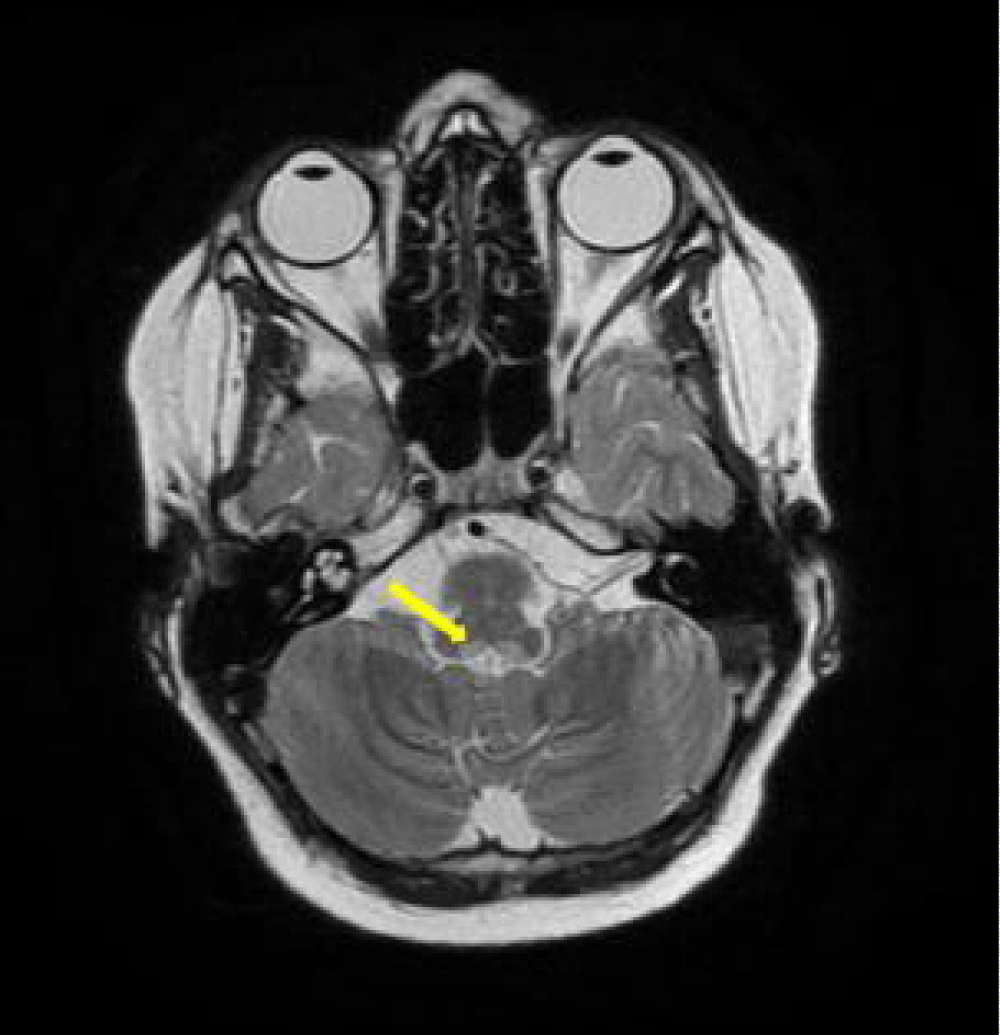
Brain magnetic resonance imaging shows a defined T2 hyperintense area in the periaqueductal region (Figure 3).
Figure 3: Axial T2-weighted magnetic resonance image with hyperintense areas in the periaqueductal region (yellow arrow).
A lumbar puncture was performed with pressure measurement and it was normal.
Laboratory investigations, including complete blood count, erythrocyte sedimentation rate, C reactive protein, fasting blood sugar, and kidney function tests were all within the normal range. A serum electrolyte typically shows hypernatremia. Furthermore, a high value of antitransglutaminase antibodies (AntiTG IgA and AntiTG IgG) was disclosed.
We have concluded that unknown celiac disease was liable for Wernicke encephalopathy.
The severity of the disease made that the supplementation should be anticipated without waiting for the thiamine results. However, the patient refuses any parenteral form. Therefore, he was given oral Thiamine 200 mg, three times/day.
The patient was also followed in the gastro-enterology pediatric department for his celiac disease.
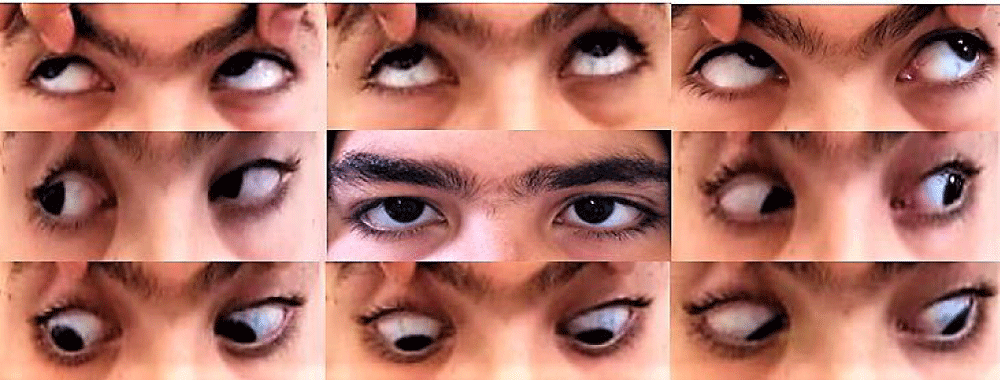
Within two weeks, diplopia, and lateral rectus palsies began to improve, his ataxic gait disappeared completely but nystagmus remains persistent (Figure 4). Whole-blood thiamine level, repeated after supplementation, was normal (83nmol/L versus 41 nmol/L before).
Figure 4: After treatment, the examination shows normal ocular motility.
He remains well on follow-up at 1 month, with a normal Lancaster test (Figure 5).
Figure 5: After treatment, the examination shows normal ocular motility.
Wernicke’s encephalopathy is a result of thiamine deficiency, mostly associated with chronic alcoholism. It can also be included in other causes, such as the surgical treatment of gastrointestinal diseases [4], hyperemesis gravidarum [5], acquired immunodeficiency syndrome (AIDS) [1], Crohn’s disease [4], anorexia nervosa [1], malnutrition and unbalanced diets [4].
In our case, uncontrollable vomiting and signs of celiac disease caused vitamin depletion in the patient.
Typically, the syndrome comprises changes in mental state, gait ataxia, and ophthalmoplegia [6]. However, the full triad has been rarely described [6]. In fact, the major ophthalmological signs in WE comprise abduction paresis, horizontal and vertical gaze palsy, internuclear ophthalmoplegia, horizontal and vertical nystagmus, and optic neuropathy [5]. Our patient presented with bilateral abduction palsy, up-beating nystagmus, and gait ataxia.
The brain MRI has outcomes in diagnosis and follow-up examinations to monitor prognosis. Particular damage in the thalamus, especially medial and intralaminar nuclei, inferior colliculus, and other vulnerable areas has been discerned, where thiamine is processed [4].
In the present case, the periaqueductal region was abnormal which was correlated with the clinical findings.
WE remains a clinical diagnosis and a medical emergency, that should be treated immediately. Treatment should not wait or be based on laboratory or imaging results [1]. That being said, if treated correctly ophthalmological signs begin to improve gradually. Nystagmus and ocular motility abnormalities can be recovered in 1-2 weeks. However, gait disorders may endure in up to 60% and just 20% of cases have entirely memory rehabilitation [7].
Bilateral Ocular motility disorders, gait instability, and nystagmus should raise the suspicion of WE, especially when there is a predisposition. Thiamine dosage and brain MRI help with diagnosis. Nevertheless, immediate treatment is crucial and can prevent sequelae.
Authors’ contributions
All the authors contribute to the management of this case and the redaction of this manuscript. All the authors have given their approval to the final version of the manuscript.
Ethical considerations
The authors declare that they have the patient’s consent to appear in a journal article.
- Theodoreson MD, Zykaite A, Haley M, Meena S. Case of non-alcoholic Wernicke's encephalopathy. BMJ Case Rep. 2019 Nov 14;12(11):e230763. doi: 10.1136/bcr-2019-230763. PMID: 31732541; PMCID: PMC6887470.
- Ota Y, Capizzano AA, Moritani T, Naganawa S, Kurokawa R, Srinivasan A. Comprehensive review of Wernicke encephalopathy: pathophysiology, clinical symptoms and imaging findings. Jpn J Radiol. 2020 Sep;38(9):809-820. doi: 10.1007/s11604-020-00989-3. Epub 2020 May 10. PMID: 32390125.
- Lebwohl B, Rubio-Tapia A. Epidemiology, Presentation, and Diagnosis of Celiac Disease. Gastroenterology. 2021 Jan;160(1):63-75. doi: 10.1053/j.gastro.2020.06.098. Epub 2020 Sep 18. PMID: 32950520.
- Liang H, Wu L, Liu LL, Han J, Zhu J, Jin T. A case report: Non-alcoholic Wernicke encephalopathy associated with polyneuropathy. J Int Med Res. 2017 Dec;45(6):1794-1801. doi: 10.1177/0300060517699039. Epub 2017 Apr 3. PMID: 28367669; PMCID: PMC5805199.
- Hokazono K, Geminiani F, Bertholdo D. Acute up-beating nystagmus in a pregnant woman with hyperemesis gravidarum. Am J Ophthalmol Case Rep. 2017 Mar 14;6:81-83. doi: 10.1016/j.ajoc.2017.01.008. PMID: 29260066; PMCID: PMC5722145.
- Fujikawa T, Sogabe Y. Wernicke encephalopathy. CMAJ. 2020 Feb 10;192(6):E143. doi: 10.1503/cmaj.190998. PMID: 32041699; PMCID: PMC7012630.
- Ong C, Patel K, Musiek E, Van Stavern G. Mystery case: a young woman with isolated upbeating nystagmus. Neurology. 2015 Jan 27;84(4):e17-9. doi: 10.1212/WNL.0000000000001178. PMID: 25628435.