More Information
Submitted: May 05, 2025 | Approved: May 22, 2025 | Published: May 23, 2025
How to cite this article: Rathi A, Gill S, Chauhan RS, Deswal J, Sagar A, Rathi N. Impact of Refractive Error Correction on Vision Related Quality of Life in School-Aged Children-A Prospective Interventional Study. Int J Clin Exp Ophthalmol. 2025; 9(1): 011-017. Available from:
https://dx.doi.org/10.29328/journal.ijceo.1001061.
DOI: 10.29328/journal.ijceo.1001061
Copyright Licence: © 2025 Rathi A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: URE; VRQoL; QoL; SREEQ
Impact of Refractive Error Correction on Vision Related Quality of Life in School-Aged Children-A Prospective Interventional Study
Ashok Rathi*, Sonam Gill, RS Chauhan, Jyoti Deswal, Abhishek Sagar and Nipun Rathi
Professor, Regional Institute of Ophthalmology, Pt. B.D.Sharma, Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India
*Address for Correspondence: Dr. Ashok Rathi, Professor, Regional Institute of Ophthalmology, Pt. B.D.Sharma, Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India, Email: [email protected]
Aim: To compare the vision related quality of life before and after prescription of refractive glasses in school-aged children.
Design: A prospective, comparative, and hospital-based interventional study was conducted at the Regional Institute of Ophthalmology, PGIMS, Rohtak between May 2021-May 2022. It involved assessment of vision-related quality of life (VRQoL) in 200 school-going children of the 5-16 age group, then comparing outcomes in children with URE versus those corrected with eyeglasses. Those with significantly low visual acuity (≤ 6/9) on Snellen’s were enrolled in the study after obtaining written informed consent from parents. The Modified SREEQ was used to assess VRQoL. Various parameters of comparison included age, gender, demography, education, and improvement in VRQoL within individual study groups over time. Comparison was done before and after using prescription refractive eyeglasses with a follow-up period of 3 months.
Results: The correction amongst hypermetropes, 40 out of total 200 students (20%), correction among myopes (153 of 200 students), correction amongst students with astigmatism (7 out of 200 students) resulted in changing categories from mild/moderate/severe visual impairment to normal category of visual acuity i.e., 6/6 on immediate correction with refractive glasses prescribed to them post refraction. Students with astigmatism showed an improvement in symptoms like distorted images post-refractive correction at 3 months. Thus, proving a positive role of refractive eyeglasses in reducing the burden of refractive errors in our study population and improving the visual outcome.
Conclusion: VRQoL was better in students after they got their refractive errors corrected with prescription eyeglasses at 3 months as compared to their QoL evaluated at their first visit to our centre with URE. This study focused on having a holistic approach towards improvement in QoL by taking into consideration the academic, psychological, cost-effectiveness aspects of VRQoL among students in the age group 5-16 years old.
Uncorrected Refractive Error (URE) is defined as a presenting visual acuity of less than 6/12 in the better eye that improves by at least 0.2 logMAR (approximately two lines on a chart) following appropriate refraction [1]. Globally, URE is a major cause of visual impairment, affecting around 259 million people, with nearly 42 million individuals classified as blind (visual acuity less than 3/60 in the better eye) [2]. Children are particularly vulnerable to Refractive Errors (RE), because even minor visual deficits can significantly interfere with their educational progress, social interactions, and overall prospects [3,4]. Moreover, while the standard treatment for RE is the provision of corrective spectacles, some studies have noted that wearing glasses may negatively impact children’s self-esteem [5,6] and increase the risk of bullying [7].
Over the past two decades, the epidemiology and distribution of refractive errors in children have drawn increasing attention. However, an important aspect that has received limited exploration is the impact of URE on vision-related quality of life (VRQoL). Quality of life (QoL), as defined by the World Health Organization (WHO), is the individual’s perception of their position in life relative to their cultural context, goals, expectations, and concerns [8]. VRQoL applies this concept specifically to issues arising from visual impairment. Although multiple instruments exist for evaluating VRQoL, few are designed specifically for children, and even fewer adequately assess the impact of refractive errors [9,10]. While instruments such as the Children’s Visual Function Questionnaire [11] and the Impact of Vision Impairment on Children Instrument have been validated for significant non-correctable visual impairment, they are less suited for URE.
In response to this gap, several questionnaires have been developed to evaluate VRQoL related to RE in adults, such as the NEI-RQL-42 [12], RSVP [13], Quality of Vision questionnaire, VRQoL [14], and the QIRC [15]. However, most are inappropriate for the pediatric population. The only instrument previously found to be suitable for children was the Pediatric Refractive Error Profile (PREP) [16,17], but it lacked comprehensive psychometric validation and was designed to detect differences between spectacle and contact lens correction [18]. “This gap led to the creation of the Student Refractive Error and Eyeglasses Questionnaire (SREEQ), designed specifically for school-aged children. This study was designed to assess the impact of URE on VRQoL and to evaluate the improvement in quality of life after the correction of refractive errors using prescription eyeglasses.
This was a one-year, prospective, comparative, hospital-based interventional study conducted at the Regional Institute of Ophthalmology (RIO), Pt. B.D. Sharma PGIMS, Rohtak. The study population consisted of 200 children between 5 and 16 years of age diagnosed with refractive errors. In order to capture age-related differences, the subjects were divided into three distinct groups: 5 – 8 years, 9 – 12 years, and 13 – 16 years. These groupings were further aligned with their respective levels of schooling: primary, secondary, and senior secondary, which also allowed an evaluation of the potential impact of educational level on VRQoL.
Upon enrolment, each participant’s demographic data was recorded. Visual acuity was assessed binocularly using the Snellen visual acuity chart—first without correction, then using a pin-hole, and finally after a refraction assessment. Best-Corrected Visual Acuity (BCVA) was determined using both objective and subjective methods. These measurements were classified according to the International Classification of Diseases (ICD)-11, which categorizes levels of visual impairment ranging from mild to severe, including blindness. Refraction procedures, including both automated refraction and retinoscopy, were performed both with and without cycloplegics (1% atropine for cycloplegia).
For the assessment of VRQoL, the SREEQ was administered in two parts. Part A consisted of 38 statements that captured the children’s perceptions regarding their uncorrected vision at their initial visit, with questions framed to reflect experiences “when I don’t wear my glasses.” Each response was scored on a four-point scale: A score of 1 was given if the symptom was experienced “all the time,” 2 for “most of the time,” 3 for “some of the time,” and 4 for “none of the time.” Part B of the questionnaire assessed the children’s perceptions after refractive correction (Table 1). Initially, Part B was administered on day 0, immediately after refraction, to assess any immediate changes in visual acuity. However, since many responses only captured short-term improvements, a more comprehensive reassessment was conducted at the 3-month follow-up. During this follow-up, Part B was re-administered to assess long-term improvements in both visual function and quality of life.
| Table 1: Following table shows questions which were comparable amongst the two parts i.e., part A and B. The second half of the table shows responses to the questions which were present only in part A. The third half of the table shows responses to part B as they could be observed only post refractive correction. |
|||||||
| Age (years)→ | 5 – 8 Years | 9 – 12 Years | 13 – 16 Years | ||||
| Question | mean | ± sd | mean | ±sd | mean | ±sd | |
| When I don’t wear my glasses, I have problems seeing clearly | Pre | 2.00 | ±0 | 2.00 | ±0 | 2.00 | ±0 |
| Post | 4.00 | ±0 | 4.00 | ±0 | 4.00 | ±0 | |
| p - value | - | - | - | ||||
| When I don’t wear my glasses, my vision is very clear | Pre | 4.00 | ±0 | 4.00 | ±0 | 4.00 | ±0 |
| Post | 1.98 | ±0.15 | 2.00 | ±0 | 2.00 | ±0 | |
| p - value | <0.001 | - | - | ||||
| When I don’t wear my glasses, my vision is blurry. | Pre | 2.00 | ±0 | 2.00 | ±0 | 2.00 | ±0 |
| Post | 4.00 | ±0 | 4.00 | ±0 | 4.00 | ±0 | |
| p - value | - | - | - | ||||
| When I don’t wear my glasses, I have to squint to see things clearly. | Pre | 3.00 | ±0 | 3.00 | ±0 | 3.00 | ±0 |
| Post | 4.00 | ±0 | 4.00 | ±0 | 4.00 | ±0 | |
| p - value | - | - | - | ||||
| When I don’t wear my glasses, I have problems seeing the computer or video games clearly. | Pre | 2.00 | ±0 | 2.00 | ±0 | 2.00 | ±0 |
| Post | 4.00 | ±0 | 4.00 | ±0 | 4.00 | ±0 | |
| p - value | - | - | - | ||||
| When I don’t wear my glasses, I have problems reading. | Pre | 2.00 | ±0 | 2.00 | ±0 | 2.00 | ±0 |
| Post | 4.00 | ±0 | 4.00 | ±0 | 4.00 | ±0 | |
| p - value | - | - | - | ||||
| When I don’t wear my glasses, I am able to see clearly far away | Pre | 4.00 | ±0 | 3.99 | ±0.11 | 4.00 | ±0 |
| Post | 1.00 | ±0 | 1.00 | ±0 | 1.00 | ±0 | |
| p - value | - | <0.001 | - | ||||
| When I don’t wear my glasses, I have problems seeing the board, at the movies, or other things far away. | Pre | 2.00 | ±0 | 2.00 | ±0 | 2.00 | ±0 |
| Post | 4.00 | ±0 | 4.00 | ±0 | 4.00 | ±0 | |
| p - value | - | - | - | ||||
| Age (years)→ Question |
5 – 8 | Years | 9 - 12 | Years | 13 - 16 | Years | |
| mean | ± sd | mean | ±sd | mean | ±sd | ||
| When I don’t wear my glasses, I have problems recognizing people across the street or down the hall. | Pre | 2.00 | ±0 | 2.01 | ±0.11 | 2.00 | ±0 |
| Post | 4.00 | ±0 | 4.00 | ±0 | 4.00 | ±0 | |
| p - value | - | <0.001 | - | ||||
| When I don’t wear my glasses, I get headaches or my head or eyes hurt when I read | Pre | 2.00 | ±0 | 2.00 | ±0 | 2.00 | ±0 |
| Post | 4.00 | ±0 | 4.00 | ±0 | 4.00 | ±0 | |
| p - value | - | - | - | ||||
| When I don’t wear my glasses, things look distorted, slanted or double. | Pre | 2.00 | ±0 | 2.00 | ±0 | 2.00 | ±0 |
| Post | 3.02 | ±0.15 | 3.00 | ±0 | 3.00 | ±0 | |
| p - value | <0.001 | - | - | ||||
| When I don’t wear my glasses, I feel dizzy. | Pre | 3.00 | ±0 | 3.00 | ±0 | 3.00 | ±0 |
| Post | 3.00 | ±0 | 3.00 | ±0 | 3.00 | ±0 | |
| p - value | - | - | - | ||||
| When I don’t wear my glasses, I have problems seeing things when I play outdoors. | Pre | 2.00 | ±0 | 2.00 | ±0 | 2.00 | ±0 |
| Post | 3.00 | ±0 | 3.00 | ±0 | 3.00 | ±0 | |
| p - value | - | - | - | ||||
| When I don’t wear my glasses, my schoolwork is harder to do | Pre | 2.98 | ±0.15 | 3.00 | ±0 | 3.00 | ±0 |
| Post | 1.00 | ±0 | 1.00 | ±0 | 1.00 | ±0 | |
| p - value | <0.001 | - | - | ||||
| When I don’t wear my glasses, it is harder to do well on tests | Pre | 2.00 | ±0 | 2.00 | ±0 | 2.00 | ±0 |
| Post | 1.00 | ±0 | 1.00 | ±0 | 1.00 | ±0 | |
| p - value | - | - | - | ||||
| When I wear my glasses, my nose or ears hurt | Pre | 3.00 | ±0 | 3.00 | ±0 | 3.00 | ±0 |
| I am bothered by my glasses when I play sports, dance or do other activities. | Pre | 3.00 | ±0 | 3.00 | ±0 | 3.00 | ±0 |
| Age (years)→ Question |
5 – 8 | Years | 9 - 12 | Years | 13 - 16 | Years | |
| When I wear my glasses, my classmates make fun of me | Post | 3.00 | ±0 | 3.00 | ±0 | 3.00 | ±0 |
| When I wear my glasses, I like how I look | Post | 2.24 | ±0.43 | 2.19 | ±0.4 | 2.18 | ±0.38 |
| I like my frames | Post | 2.00 | ±0 | 2.00 | ±0 | 2.00 | ±0 |
| If I didn’t wear glasses, I would look better | Post | 2.76 | ±0.43 | 2.81 | ±0.4 | 2.83 | ±0.38 |
| When I wear my glasses, my friends like the way I look | Post | 2.00 | ±0 | 2.00 | ±0 | 2.00 | ±0 |
| When I wear my glasses, my family members like the way I look | Post | 1.00 | ±0 | 1.00 | ±0 | 1.00 | ±0 |
Data analysis included summarizing frequency distributions with supporting graphs, and quantitative variables were expressed as mean ± Standard Deviation (SD). Comparisons between groups were made using ANOVA and unpaired t - tests, and within-group differences over time were analyzed using paired t-tests. A p - value of less than 0.05 was considered statistically significant.
The study population was divided into three age groups: 5 – 8 years, 9 – 12 years, and 13 – 16 years. The mean ages for these groups were 6.65 ± 0.95, 10.85 ± 1.01, and 14.23 ± 1.01 years, respectively. Gender-specific analyses showed similar distributions, with only minor variations between male and female children.
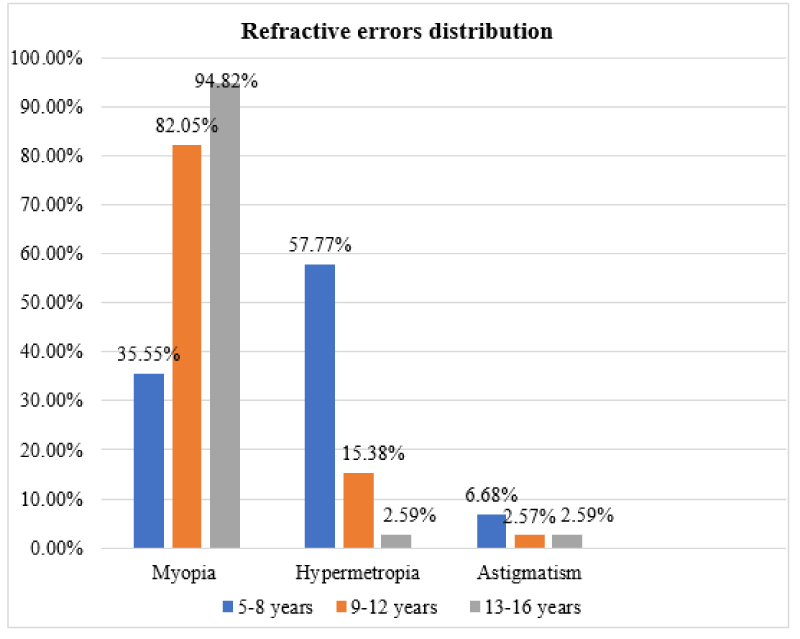
Age wise distribution of the refractive errors showed that Myopia was found to be more prevalent in older age groups with a percentage of 82.05% in 9 - 12 age group and 94.82% in 13-16 age group. On the other hand, Hypermetropia was found to be more prevalent in younger age group i.e., 5-8 years old with a percentage of 57.77% (compared to Myopia prevalence of 35.55% in that same age group. Astigmatism was found to be more prevalent among the age group of 5 - 8 years old (6.68%). Its prevalence among 13-16 years old was equivalent to that of Hypermetropia in the same group i.e., 2.59% (Figure 1).
Figure 1: Showing percentage of myopia, hypermetropia and astigmatism across different age groups.
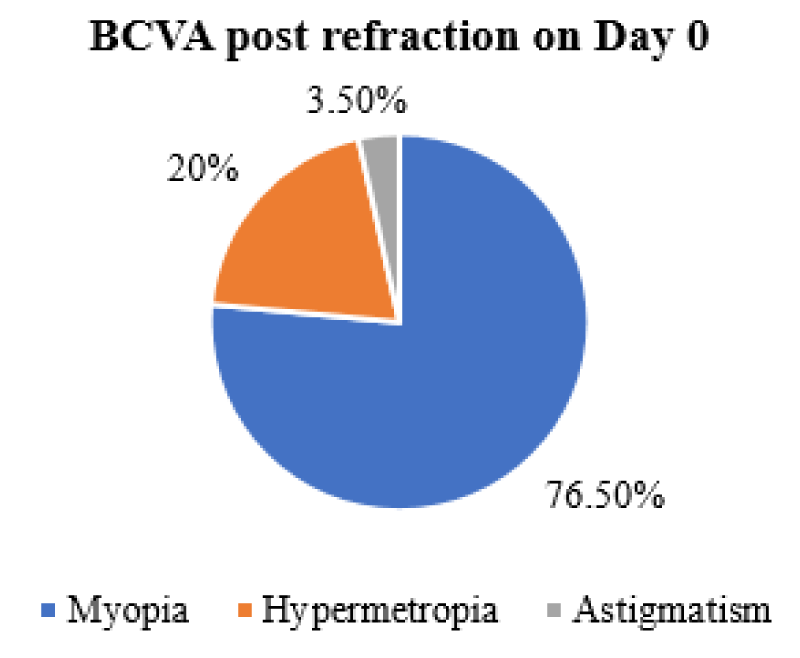
At the initial visit (pre-refraction), all 200 subjects completed Part A of the SREEQ, capturing their baseline perceptions of uncorrected vision. Following refractive correction on day 0, all participants experienced an immediate improvement in visual acuity, achieving 6/6 vision with myopic correction in 76.5%, hypermetropia in 20% and astigmatism in 3.5% children (Figure 2). In 153 myopic students, this correction resulted in a significant shift in their ICD-11 classification from categories of mild, moderate, or severe visual impairment (or blindness) to a normal visual status. While this immediate improvement was significant, the full impact of spectacle correction on daily functioning, academic performance, and psychosocial well-being could only be thoroughly assessed at the 3-month follow-up.
Figure 2: Showing BCVA post- refraction on Day-0.
At the 3-month evaluation, all students underwent a repeat detailed eye examination, including refraction, to verify the stability of the correction. The post-correction responses (Part B) were then compared with the baseline data (Part A). The findings were consistent across different refractive errors: among 153 myopes, 40 hypermetropes, and 7 astigmatic children, the majority maintained a BCVA of 6/6. This sustained improvement not only highlighted the long-term benefits of spectacles in enhancing visual acuity but also demonstrated significant improvements in overall VRQoL.
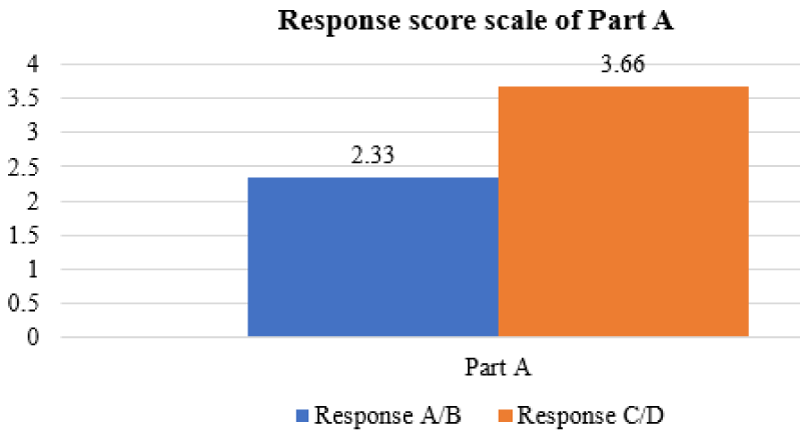
Pre-correction (Part A) responses detailed high frequencies of symptoms such as high frequencies of visual symptoms, including blurry vision, difficulty focusing, eye strain, and headaches. Questions related to blurry vision, squinting, difficulty in reading, recognizing faces at a distance, and eye pain were answered predominantly with scores indicating that these issues occurred “all” or “most of the time.” This pattern was particularly marked in those classified under moderate to severe visual impairment according to ICD-11, where the mean scores were approximately 2.33 ± 0.1 (p < 0.001), indicating significant visual and functional challenges faced by these children in daily activities, academic performance, and even extracurricular tasks such as playing sports (Figure 3).
Figure 3: Represents the mean value of responses of score scale of Part-A of SREEQ.
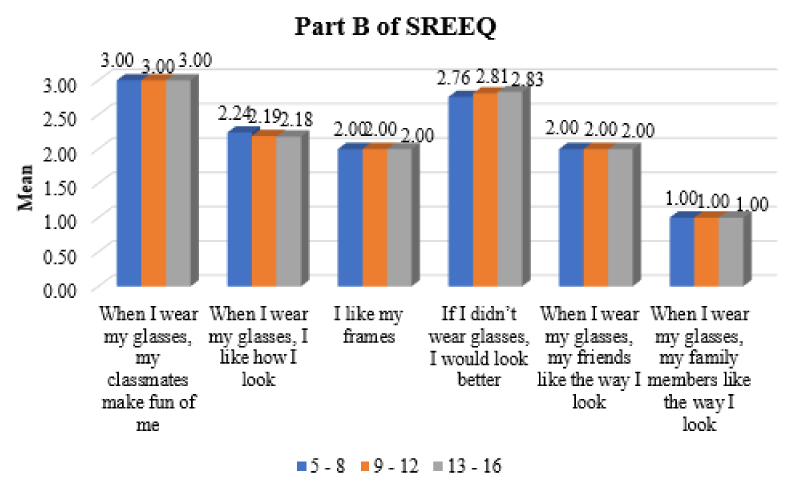
At follow-up, the corresponding questions in Part B (phrased in the context of “when I wear my glasses”) showed a dramatic improvement. For example, questions on clear distance vision, ease of reading, and improved test performance showed scores with means of 1 to 2, again with statistically significant differences (p < 0.001). Additionally, while some questions—particularly those related to the psychosocial impact of wearing glasses—still reflected some level of discomfort or self-consciousness (e.g., feelings of physical discomfort or concerns about appearance), the overall trend was one of marked improvement in quality of life (Figure 4).
Figure 4: Represents the mean value of responses of score scale of Part-B of SREEQ.
The study also analyzed differences in responses based on ICD-11 visual impairment categories. In children with moderate to severe impairment, the benefits of spectacle correction were most pronounced, with significant improvements in daily functioning and academic performance. In contrast, children with relatively milder impairments (those who initially reported clearer vision even without correction) showed less dramatic changes in some subjective aspects, such as the frequency of experiencing dizziness or the clarity of vision without glasses. Nonetheless, the data collectively underscore that appropriate refractive correction plays a crucial role in enhancing VRQoL across various domains.
The prevalence of mild visual impairment was 17.64% with Myopia and 25.0% with Hypermetropia. Moderate visual impairment due to Myopia was 26.24% and Hypermetropia was 37.5%. Severe visual impairment was mainly due to Myopia with a prevalence of 3.75%. Astigmatism resulted in mild visual impairment with a prevalence of 14.28%. According to the study by Sheeladevi S. et al, the overall prevalence of refractive error per 100 children was 8.0 (CI: 7.4 - 8.1) and in schools it was 10.8 (CI: 10.5 - 11.2). The population-based prevalence of myopia, hyperopia (≥ +2.00 D) and astigmatism was 5.3 per cent, 4.0 per cent and 5.4 per cent, respectively. But this study was done in children < 15 years and our study group ranged from 5 - 16 years [19].
The two-group design—pre-correction versus post-correction (immediate and 3-month follow-up)—allowed a comprehensive assessment of the impact of refractive error correction on quality of life. Initially, the immediate post-correction assessments (day 0) primarily reflected changes in objective visual acuity, while the 3-month follow-up provided deeper insights into how these improvements translated into better academic performance, improved participation in outdoor activities, and enhanced psychosocial well-being.
A detailed analysis of the SREEQ responses revealed that children with uncorrected refractive errors experienced significant difficulties with distant vision tasks. These difficulties were most notable in academic settings, where problems such as reading the blackboard and following visual instructions were reported. Other common complaints included blurry vision, squinting, headaches, eye strain, and even distorted vision—all of which had a direct impact on daily activities and learning.
The study’s results also highlighted a psychosocial dimension to URE. Several questions in the questionnaire were designed to assess the children’s self-perception and the perceptions of their peers and family members regarding the use of spectacles. Some teenagers reported feeling self-conscious, experiencing discomfort, or even facing teasing from peers. These negative psychosocial factors are critical as they can lead to poor compliance with spectacle wear, further exacerbating the negative impact of refractive errors on VRQoL [20,21].
Methodologically, while the SREEQ provided a useful framework for evaluating VRQoL, the study noted that Part B of the questionnaire exhibited a lower person separation index compared to Part A (0.25 vs. 0.86, respectively). The person separation index reflects how well an instrument distinguishes between different levels of ability or response variations; in this case, the lower value suggests that, once corrected, the children’s responses became more uniform due to the uniformly good visual acuity, thereby reducing the instrument’s ability to differentiate between individuals. future versions of the SREEQ may benefit from a refined possibly streamline the four-point scale into three points by merging similar responses—to enhance its sensitivity and reliability (Figure 5).
Figure 5: Represents an overview of the quality of life assessed via responses to all the questions which were corresponding to each other amongst Part A and Part B.
The study also performed a subgroup analysis based on age and educational level. Younger children (5 – 8 years) and those in primary school had different patterns of response compared to older children (13 – 16 years), particularly regarding psychosocial factors. This difference underscores the need for age-appropriate counselling and education about the importance of spectacle wear, not only for vision correction but also as a tool for overall enhancement of quality of life [22].
Additionally, a minor but notable point from the study was the observation that while the majority of children adjusted well to the new spectacles, some did report transient issues such as experienced transient headaches during the adjustment period. These issues were more prevalent among myopes with poorer uncorrected visual acuity (6/24 or worse), indicating that the severity of URE might influence the adaptation period following correction.
This study demonstrates that correcting refractive errors with prescription eyeglasses leads to significant improvements in the vision-related quality of life (VRQoL) of children aged 5 – 16 years. After a 3-month follow-up period, children exhibited not only restored to visual acuity (6/6 across all groups) but also improved performance in academic tasks and extracurricular activities. In particular, children with moderate to severe visual impairment benefited most from the intervention, shifting from classifications of visual disability to normal vision as per ICD-11 criteria.
Despite these positive outcomes, the study also identified several challenges that may contribute to the persistence of uncorrected refractive errors in the region. These include a lack of awareness regarding refractive error symptoms, limited health literacy among rural populations, social stigma and peer pressure, especially among teenagers, and issues related to initial discomfort with new glasses. These factors underscore the importance of a holistic approach when addressing URE in children, one that includes not only clinical correction but also educational, psychosocial, and community outreach components.
The findings also suggest that while the SREEQ is a promising tool for assessing VRQoL in children with refractive errors, further refinements are needed. In particular, modifying the response scale and adding specific questions regarding aesthetic and functional aspects of spectacle wear could enhance the instrument’s ability to capture subtle differences in quality of life. Future research should continue to refine these tools and explore strategies to overcome the barriers that lead to noncompliance and under correction of refractive errors.
Overall, the study confirms that early detection and correction of refractive errors are crucial. By addressing these errors through appropriate spectacle use, it is possible to improve not only the visual function but also the academic, physical, and psychosocial well-being of children—a benefits that may extend into adulthood, enhancing long-term quality of life.
- Lou L, Yao C, Jin Y, Perez V, Ye J. Global patterns in health burden of uncorrected refractive error. Invest Ophthalmol Vis Sci. 2016;57(14):6271–7. Available from: https://doi.org/10.1167/iovs.16-20242
- Ferraz FH, Corrente JE, Opromolla P, Schellini SA. Influence of uncorrected refractive error and unmet refractive error on visual impairment in a Brazilian population. BMC Ophthalmol. 2014;14(1):84. Available from: https://doi.org/10.1186/1471-2415-14-84
- Ip JM, Robaei D, Kifley A, Wang JJ, Rose KA, Mitchell P. Prevalence of hyperopia and associations with eye findings in 6- and 12-year-olds. Ophthalmology. 2008;115(4):678–85. Available from: https://doi.org/10.1016/j.ophtha.2007.04.061
- Vitale S, Cotch MF, Sperduto RD. Prevalence of visual impairment in the United States. JAMA. 2006;295(18):2158. Available from: https://doi.org/10.1001/jama.295.18.2158
- Terry RL, Brady CS. Effects of framed spectacles and contact lenses on self-ratings of facial attractiveness. Percept Mot Skills. 1976;42(3):789–90. Available from: https://doi.org/10.2466/pms.1976.42.3.789
- Terry RL, Berg AJ, Phillips PE. The effect of eyeglasses on self-esteem. J Am Optom Assoc. 1983;54:947–9. Available from: https://pubmed.ncbi.nlm.nih.gov/6630845/
- Horwood J, Waylen A, Herrick D, Williams C, Wolke D. Common visual defects and peer victimization in children. Invest Ophthalmol Vis Sci. 2005;46(4):1177–81. Available from: https://doi.org/10.1167/iovs.04-0597
- Wong HB, Machin D, Tan SB, Wong TY, Saw SM. Visual impairment and its impact on health-related quality of life in adolescents. Am J Ophthalmol. 2009;147(3):505–11. Available from: https://doi.org/10.1016/j.ajo.2008.09.025
- Nichols JJ, Mitchell GL, Saracino M, Zadnik K. Reliability and validity of refractive error-specific quality-of-life instruments. Arch Ophthalmol. 2003;121(9):1289–96. Available from: https://doi.org/10.1001/archopht.121.9.1289
- Gothwal VK, Wright TA, Elliott DB, Pesudovs K. The refractive status and vision profile: Rasch analysis of subscale validity. J Refract Surg. 2010;26(11):912–5. Available from: https://doi.org/10.3928/1081597x-20100512-01
- Felius J, Stager DR Sr, Berry PM, Fawcett SL, Stager DR Jr, Salomão SR, et al. Development of an instrument to assess vision-related quality of life in young children. Am J Ophthalmol. 2004;138(3):362–72. Available from: https://doi.org/10.1016/j.ajo.2004.05.010
- Hays RD, Mangione CM, Ellwein L, Lindblad AS, Spritzer KL, McDonnell PJ. Psychometric properties of the National Eye Institute-Refractive Error Quality of Life instrument. Ophthalmol. 2003;110(12):2292–301. Available from: https://doi.org/10.1016/j.ophtha.2002.07.001
- Vitale S, Schein OD, Meinert CL, Steinberg EP. The refractive status and vision profile: a questionnaire to measure vision-related quality of life in persons with refractive error. Ophthalmol. 2000;107(8):1529–39. Available from: https://doi.org/10.1016/s0161-6420(00)00171-8
- Brady CJ, Keay L, Villanti A, Ali FS, Gandhi M, Massof RW, et al. Validation of a visual function and quality of life instrument in an urban Indian population with uncorrected refractive error using Rasch analysis. Ophthalmic Epidemiol. 2010;17(5):282–91. Available from: https://doi.org/10.3109/09286586.2010.511756
- Pesudovs K, Garamendi E, Elliott DB. The Quality of Life Impact of Refractive Correction (QIRC) Questionnaire: development and validation. Optom Vis Sci. 2004;81(10):769–77. Available from: https://doi.org/10.1097/00006324-200410000-00009
- Khadka J, McAlinden C, Pesudovs K. Quality assessment of ophthalmic questionnaires: review and recommendations. Optom Vis Sci. 2013;90(8):720–44. Available from: https://doi.org/10.1097/opx.0000000000000001
- Walline JJ, Jones LA, Chitkara M, Coffey B, Jackson JM, Manny RE, et al. The Adolescent and Child Health Initiative to Encourage Vision Empowerment (ACHIEVE) study design and baseline data. Optom Vis Sci. 2006;83(1):37–45. Available from: https://doi.org/10.1097/01.opx.0000195566.94572.eb
- Ayanniyi AA, Adepoju FG, Ayanniyi RO, Morgan RE. Challenges, attitudes and practices of the spectacle wearers in a resource-limited economy. Middle East Afr J Ophthalmol. 2010;17(1):83–7. Available from: https://doi.org/10.4103/0974-9233.61223
- Mohammed Dhaiban TS, Ummer FP, Khudadad H, Veettil ST. Types and presentation of refractive error among individuals aged 0–30 years: Hospital-based cross-sectional study, Yemen. Adv Med. 2021;2021:5557761. Available from: https://doi.org/10.1155/2021/5557761
- Rajabour M, Kangari H, Pesudovs K, Khorrami-Nejad M, Rahmani S, Mohaghegh S, et al. Refractive error and vision-related quality of life. BMC Ophthalmol. 2024;24(1):83. Available from: https://doi.org/10.1186/s12886-024-03350-8
- Leshabane MM, Ram Pershad N, Mashiqe KP. Vision-related quality of life and associated factors in individuals with vision impairment. Afr J Prim Health Care Fam Med. 2025;17(1):94765. Available from: https://doi.org/10.4102/phcfm.v17i1.4765
- Kumaran SE, Balasubramaniam SM, Kumar DS, Ramani KK. Refractive error and vision-related quality of life in South Indian children. Optom Vis Sci. 2015;92(3):272–8. Available from: https://doi.org/10.1097/opx.0000000000000494