About Alyarmouk Teaching Hospital
Alyarmouk Teaching Hospital
Articles by Alyarmouk Teaching Hospital
Changes in intraocular pressure after ND-yag laser posterior capsulotomy
Published on: 20th May, 2020
OCLC Number/Unique Identifier: 8605488676
The Nd-Yag L has been developed in Europe since the mid-1970s [10]. Today Nd-Yag LPC has become an established procedure for after cataract. Before the Nd-Yag L came into use, the capsulotomy was done by performing a small puncture with a needle knife or 27 gauge needle, either at the time of original operation or as a secondary procedure through the limbus in aphakic or through pars plana in pseudophakic. The Nd-Yag L preferred because it is non-invasive and infection cannot occur. The most important complication is a transient rise in IOP 1-3 hrs of Nd-Yag LPC [1]. Occasionally the pressure rise is high and can cause serious damage to the optic nerve, so that the IOP should be monitored and appropriate measures should be taken if necessary. Only if we can minimize its frequency or, better still, avoid it, altogether, can we accept Nd-Yag L as a safe procedure in our effort to restore vision. In otherwise normal eyes, a mild elevation of IOP is of no consequence because it usually resolves within 24 hour especially when the patient receives anti-glaucoma drugs before and after laser application. However in eyes with pre-existing glaucoma, the incidence of IOP elevation is higher and its duration is longer than in otherwise normal eyes. Some glaucomatous eyes may therefore require additional glaucoma therapy for several weeks following Nd-Yag LPC [3]. So monitoring is particularly important in the cases of glaucoma with optic nerve damage and field loss as these eyes are susceptible to small pressure rises for even a short period. A single rise to 40mmHg for a few hours can cause irreversible damage to the damaged optic nerve and lead to permanent visual loss or even blindness [1]. The purpose of this study is to evaluate the changes in IOP at 1hour,24hour and 1 week after Nd-Yag LPC.
The evaluation of bandage soft contact lenses as a primary treatment for traumatic corneal abrasions
Published on: 25th May, 2020
OCLC Number/Unique Identifier: 8605482786
Background: Corneal abrasions are a common result of eye trauma. Corneal injuries are very common in both the adult and pediatric population and account for a significant proportion of the workload of most emergency departments. Although abrasion heals well with preservative treatment, it still causes pain and job lost. The abrasion result from the scrabble of the corneal epithelium. These injuries cause pain, tearing, lids spasm, light scare, foreign body sensation, decreased visual acuity/blurring, and a gritty feeling. The light, friction & wink was worse the condition. Most abrasion cure within 24-27 hours and seldom proceed to erosion or infection. The study aims to use bandage soft contact lens [BSCL] as a primary treatment for traumatic corneal abrasion [TCA] instead of traditionally use pressure patch [PP].
Patients and methods: The present prospective study has been conducted on 50 patients attending the out-patient department of ophthalmology in an Alyarmouk teaching hospital for six months after taking ethical permission. Before subjecting the patient to the treatment of bandage soft contact lens therapy, a detailed clinical history and thorough local examination have been done. A history indicating the occurrence of recent ocular trauma followed by severe pain, redness, lids spasm, photophobia, and tearing of the involved eye is suggestive of a corneal abrasion. Always we ask about contact lens wear as this can complicate the presence of an abrasion. To confirm the diagnosis of traumatic corneal abrasion we examine the cornea by slit-lamp under cobalt-blue filtered light after the application of tetracaine eye drops & fluorescein strips. The treatment of 50 consecutive patients presenting with traumatic corneal abrasion has been treated with anesthetic eye drop (tetracaine 0.5%) to relieve pain and lids spasm, antibiotic eye drop (ofloxacin 0.3%), therapeutic bandage soft contact lens was applied to provide pain relief and once again act as a splint to promote epithelial healing, then visual acuity was measured by Snellen chart, a cycloplegic eye drop (cyclopentolate 1%) was applied to relieve ciliary spasm & then preservative-free lubricant eye drop were applied lastly. This criterion dramatically relieves most, if not all of the pain the patient may be experiencing (which is a big plus for the patient and earns instantaneous trust), but it also allows the patient to return to work/school or any other daily activities. Patients have been evaluated after 24hours, 72hours and after 1week regarding pain, visual acuity, and complications. Though pressure patch [PP] occasionally advice in abrasion therapy, it does not assist and may prevent recovery. Employ the protective eyewear can preclude the traumatic corneal abrasion.
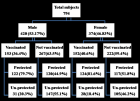
Results: A total of 50 cases were enrolled in our study during the study period of 6 months. Out of 50 patients, there were 30males and 20 females and the male/female ratio was 3:2. The patient’s age was ranged from 5-35years. The commonest cause of injury was direct minor trauma (80% of cases), with cosmetic & optical contact lenses related problems accounting for 20% of presentations, visual acuity was documented correctly in 90% of adult and pediatric group and difficult to documented in children less than 6-year-old 10%. Traumatic corneal abrasion treated with bandage soft contact lens has an apparent advantage over the traditional pressure patch in terms of reduced pain, speedier healing, and an advantage of faster rehabilitation, facilitation epithelial healing, and proper surface hydration. Evaluation of pain revealed sufficient comfort with this regimen, allowing 45 patients (90%) to go back immediately to their occupations. Moreover, visual function is retained without any complication. Healing of the traumatic corneal abrasion occurred within 1 to 3 days in all patients, with minimal or no pain. The infection did not occur at the time of the follow up. We remove the bandage soft contact lens after 1 week to allow epithelial migration and attachment without the interference of the shearing forces of the upper lid.
Conclusion: The use of bandage soft contact lens as a primary treatment for a traumatic corneal abrasion is a safe and effective method with anesthetic eye drop (tetracaine 0.5%), antibiotic eye drop (ofloxacin 0. 3%), cycloplegic eye drop (cyclopentolate 1%), preservative-free lubricant drop instead of traditionally pressure patch. Bandage soft contact lens causes dramatic improvement from pain, lid spasm, tearing & visual function is retained without any complication, and patients can immediately resume their regular activities.

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."