Table of Contents
Outcome of Trabeculectomy in Advanced Glaucoma in a tertiary hospital in Rivers State, Nigeria
Published on: 19th December, 2018
OCLC Number/Unique Identifier: 7985989438
Aim: To evaluate the outcome of Trabeculectomy in advanced glaucoma in a hospital in Rivers State, Nigeria.
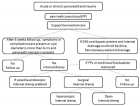
Methods: This was a non-randomized interventional study in which each patient served as its own control. Patients with advanced glaucoma and demonstrable field defects and Mean defect ≥-12 were included. The intervention employed was Trabeculectomy and IOP and visual acuity pre operative, as well as post op were collected and compared at pre- op, post -op day 1, one week, one month, 6 months. Data was analyzed using SPSS version 20.
Results: Thirteen (13) eyes from ten (10) patients with advanced glaucoma were involved in the study. Mean age of study population was 53±19.62 years. Mean of mean defect was -19.05±5.23dB while mean of vertical cup disc ratio (VCDR) was 0.88±0.04.
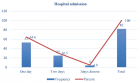
Mean of Pre- op Visual acuity (log MAR) was 0.46 and dropped to 0.72 first day post-op but improved over 6 months to 0.42. The mean of IOP pre-op was 24.15mmHg and dropped to 11.23mmHg (58.24%) over 6 months (p=0.001).
Conclusion: Trabeculectomy still remains the gold standard surgical treatment for glaucoma. In our study it resulted in a 58.24% drop in IOP over 6 months with mean visual acuity maintained at pre-op levels after 6 months follow up. It therefore is effective and safe surgical intervention in advanced glaucoma.
Is community based case detection of glaucoma relevant? Intraocular Pressure level and vertical Cup Disc ratio of participants at a screening programme in a rural setting in Nigeria
Published on: 12th November, 2018
OCLC Number/Unique Identifier: 7929242578
To determine the proportion of participants with elevated intraocular pressure and abnormal vertical cup disc ratio in a glaucoma screening event in a rural community in Nigeria.
Methods: 242 eyes of 121 participants at a one-day screening programme were examined. Visual acuity was accessed using Snellen literate and illiterate charts, followed by a pen torch examination of the anterior segment. The posterior segment was accessed using a direct ophthalmoscope (Welch Allyn, USA). All participants had intraocular accessed using Keeler non contact tonometer and those with significant media opacity preventing view of the posterior pole had cycloplegic examination after dilatation with 1%Tropicamide drops. Data generated was expressed as percentages and means.
Results: 121 participants (242 eyes) were examined. There were 42 males and 79 females giving a M:F ratio of 1:1.86. Age range of participants was 0-90years with a peak in the 5th decade. Mean age was 32 years. 79.3% of participants had normal visual acuity of 6/4 -6/18, while 9.5% had visual acuity worse than 6/60.
83% of eyes had intraocular pressure within normal level, <21mmHg, 12.4% within 21-30mmHg and 4.6% >30mmHg.
73.1% of eyes had Vertical Cup disc ratio (VCDR) <0.5, 10.7% had 0.5-0.7 and 6.6%>0.7. 9.6% of eyes could not be accessed due to media opacities.
Conclusion: 6.6% of participants had suspicious discs and 4.6% participants had intraocular pressures above 30mmHg. Opportunistic screening for glaucoma remains one of the important modes of case detection for glaucoma in the developing climes and should be encouraged as a way to address the scourge of this blinding disease.
Chronic recurrent bilateral granulomatous iridocyclitis in an 18-year-old woman
Published on: 31st July, 2018
OCLC Number/Unique Identifier: 7814922520
Ocular changes and disorders associated with Obesity
Published on: 27th July, 2018
OCLC Number/Unique Identifier: 7795938194
Obesity is a chronic and metabolic disease with a high increasing prevalence worldwide. It has multifactorial pathogenesis including genetic and behavioral factors [1-5]. Overweight and obesity have been defined and classified by the World Health Organization (WHO) and the National Institutes of Health (NIH) [2,3]. A person with a normal weight has Body Mass Index (BMI) of 18.5-24.9. A person with a BMI under 18.5 is called underweight. An adult having a BMI of 25-29.9 is overweight and pre-obese. Class 1 obesity is defined as a BMI between 30.00-34.99. Class 2 (Severe) Obesity is to have a BMI between 35.00-39.99. Morbid (Extreme, Class 3) obesity is to have a BMI over 40 [1-5]. Obesity is significantly associated with enhanced morbidity and mortality rates. It has also various economic, medical and psychological effects and causes health problems including many systemic diseases, economic costs and burdens, social and occupational stigmatization and discrimination and productivity loss [4-6]. Obesity carries the increased risk of development of many systemic and chronic diseases, including sleep apnea, depression, insulin resistance, Type 2 (adult-onset) diabetes, Gout and related arthritis, degenerative arthritis, hypertension, dyslipidemia, heart disease such as myocardial infarction, congestive heart failure, or coronary artery disease, polycystic ovary syndrome and reproductive disorders, Pickwickian syndrome (obesity, red face and hypoventilation), metabolic syndrome, non-alcoholic fatty liver disease, cholecystitis, cerebrovascular accident, colonic and renal cancer, rectal and prostatic cancer in males, and gallbladder, uterus and breast cancer in females [6-12].
In recent years, some publications reported that obesity has been strongly associated with some ocular diseases including age-related cataract and maculopathy, glaucoma, and diabetic retinopathy [13-16].
The recent reports demonstrated that the central corneal thickness and intraocular pressure were increased while as mean thickness of RNFL and retinal ganglion cell and choroidal thickness (CT) were decreased in the morbidly obese subjects [17-19]. However, another study has reported that CT increased in obese children [20]. On the other hand, a recent study reported that all values of the specific tests used to evaluate the ocular surface were within the normal range [21]. In some experimental studies, it has been demonstrated that obesity may cause retinal degeneration [22,23]. Additionally, in a past meeting presentation, it has been speculated that keratoconus is associated with severe obesity [24]. Teorically, idiopathic intracranial hypertension, and papilledema may also be associated with obesity [25]. Obesity may be also a cause of mechanical eyelid abnormalities such as entropion [26]. However, further investigations are needed to detect the significant relationship between these diseases and obesity.
On the other hand, the ocular surgeries of obese patients are difficult compared to normal weight-subjects. The posterior capsule rupture and vitreous loss may easily develop during cataract surgery of these patients because obese patients have an elevated vitreous pressure and operating table cannot often be lowered or surgeon’s chair cannot be elevated sufficiently to provide the clear viewing of the operating area and tissues. So, some different surgical manipulations such as standing phacoemulsification technique and reverse Trendelenburg position have been developed. Additionally, the standing vitrectomy technique has been used for vitreoretinal interventions in morbidly obese patients [27,28].
In conclusion, all obese subjects should be subjected to a completed ophthalmological examination and to relevant clinics for the detection of possible comorbidities and diseases

HSPI: We're glad you're here. Please click "create a new Query" if you are a new visitor to our website and need further information from us.
If you are already a member of our network and need to keep track of any developments regarding a question you have already submitted, click "take me to my Query."